In Parts 1 & 2 we looked at what Dr McDougall 1 and Dr Greger 2 have to say on the subject of CKD (chronic kidney disease) and kidney health in general. Part 3 will consider the thoughts of Dr Dean Ornish’s medical/research team.

Dr Ornish’s Preventive Medicine Research Institute (PMRI) runs a Lifestyle Medicine Program 3 which aims to treat a wide range of chronic diseases by dealing with four areas:
- diet
- stress
- exercise, and
- social interaction
Dr Ornish is an internationally respected doctor who, along with his team, have published landmark papers 4 on his successes at reversing heart disease and other diseases without the need for medications or invasive surgical procedures but, rather, by simply managing and changing the diets and lifestyles of his patients. But what does the Ornish team have to say about kidney disease?
To answer this, we’ll look at an article 5 written by one of his team of experts, Carra Richling RD 6 .

“A comprehensive low-fat, plant-based [diet] can be beneficial in both preserving and improving the function of your kidneys.”
What causes kidney disease?
Most common causes:
- diabetes
- high blood pressure
other risk factors:
- family history
- inherited diseases (e.g. polycystic kidney disease)
- kidney stones
- recurrent urinary infections
- autoimmune disorders
- inflammatory diseases
- excess amounts of phosphate (an additive in processed foods)
Plant-based diet and kidney disease
Early detection of CKD is very important in being able to successfully manage the disease most effectively.
Kidney function can be preserved and improved by adopting a low-fat, plant-based approach. A 2015 study 7 considered that: “Plant protein intake is associated with lower production of uremic toxins and lower serum phosphorus levels. Therefore, at a given total protein intake, a higher proportion of dietary protein from plant sources might be associated with lower mortality in chronic kidney disease.”
It’s also important to manage your blood pressure and blood sugars in order to maintain kidney health. [Eating a WFPB diet (with no added salt, oil or sugar) will provide the best dietary means of managing both of these.]
If you have CKD, it’s important to consult your doctor before making any dietary changes, and to work closely with your doctor/medical team by obtaining the necessary biometrics (blood pressure, blood sugar, etc), especially if you have later stages of CKD. [Having said this, there’s a real problem with achieving this when almost all conventional doctors have very little education in nutritional science and, thus, tend to defer to immediate pharmaceutical solutions. The latter often merely treat symptoms rather than the main cause – diet – and come with their own side-effects. 8 ]
Phosphorus and Your Kidneys
A phosphate is a salt containing the mineral phosphorus. Phosphorus is found in protein foods (both animal and plant). There’s an important homeostatic balance within the body between calcium and phosphorus 9 . When kidney function declines, phosphorus levels can build up to excess. Calcium deposits can then build up in the kidneys, heart valves, muscles and other parts of the body. Plant protein does not absorb phosphorus in the same way as animal protein.
A 2011 study 10 confirmed that a vegan diet produced lower phosphorus levels compared with a meat-based diet. Phosphorus in plant foods was shown to be less bioavailable than the phosphorus in animal foods. The positive result of this is that the lower absorption from plant foods limits the phosphorus load on the kidneys, thus reducing the risk of complications caused by excess phosphorus (heart disease, diabetes, and further kidney decline caused by vascular calcification). The researchers concluded that: “…the source of protein has a significant effect on phosphorus homeostasis in patients with CKD. Therefore, dietary counseling of patients with CKD must include information on not only the amount of phosphate but also the source of protein from which the phosphate derives.”
A 2010 study 11 revealed that kidney function declines in diets higher in animal protein, animal fat, and cholesterol and kidney function improves with those who followed a plant-based approach.
A 2012 study 12 on the dangers of phosphates in processed foods, came to a rather blunt conclusion: “ In view of the high prevalence of CKD and the potential harm caused by phosphate additives to food, the public should be informed that added phosphate is damaging to health. Furthermore, calls for labeling the content of added phosphate in food are appropriate.”
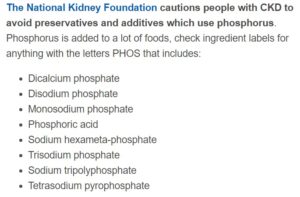
For those with CKD, eating processed foods is not a sensible idea. Phosphates, which contains phosphorus, are often added to processed foods including dairy, cereals, and soda. Indeed, healthy individuals can quickly end up with CKD by consuming high levels of processed foods.
Phosphates have to be listed on nutrition labels, so it is important to read the ingredients on packaged foods and beverages to look for hidden sources of phosphate (e.g. phosphoric acid and sodium phosphate). Artificial phosphate is absorbed differently from naturally occurring phosphate (phosphorous) and can contribute to excess amounts in the bloodstream, leading to complications, particularly in people with later stages of CKD.

Limiting Sodium, Potassium, and Phosphorus
It may be that your doctor will recommend that you lower sodium, phosphorus and potassium content in the foods you eat. This will depend, to some extent, on the stage of CKD. Sodium is always going to be less in whole plant foods than in any processed and packaged food. [Cutting out added salt is a good idea for everyone, irrespective of whether or not you have diagnosed CKD. In a previous blog 13 we looked at some great salt alternatives that can be used in your cooking. Ornish Living also provides an article 14 on which spices can be used as effective replacements for salt, as well as providing some healthy and tasty recipes.
It’s useful to become aware of which plant-based foods that are high in phosphorus such as whole grains, bran cereals, wheat germ, beans and dried peas, soy and cocoa. If you have later stage CKD, your doctor or renal dietitian may provide you with specific recommendations for limiting phosphorus, potassium and sodium. You can avoid sodium by cutting out all processed and packaged foods. We looked previously at high 15 and low 16 potassium plant foods.
Some foods low in phosphorus
The USDA Food Composition Databases provide 17 a really comprehensive list of foods by nutrient content. The latter link takes you to a page showing phosphorus, potassium and sodium content in 1000’s of individual foods.
Stage 4 CKD & WFPB diet
Another article 18 worth mentioning is written by one of the Ornish team, Dr Ben Brown, Medical Director of Ornish Lifestyle Medicine.

The article is entitled “I was Diagnosed with Stage 4 Chronic Kidney Disease. Can Ornish Lifestyle Medicine Help Control CKD?” The answer Dr Brown gives is simple: “yes, most of the time“.
“Most chronic diseases, including CKD, have a component to them that can only be treated with changes to your lifestyle.”
“Most treatments [for CKD] focus on contributing factors (smoking, hypertension, high cholesterol,diabetes, etc). Treating these risk factors with medicines alone, however, does not generally stop the progression of the disease. It just slows it down. There are other factors that lifestyle is more effective at treating than medications. These include systemic inflammation and poor nutritional states.”
In all stages of CKD the degree of reversibility with lifestyle changes depends on two factors:
- the main cause of the kidney disease
- the degree of scarring that’s already occurred
Both of these can be measured by decreased renal function (increased BUN and creatinine) and leaking of protein (albuminuria or proteinuria).
Understanding scarring of the kidneys
If pressure, inflammation and sugar damage on the tiny vessels within the kidneys goes on long enough, the blood supply to the individual kidney cell stops, the cell stops functioning, dies and creates a small scar.
Changes related to scarring are more difficult to reverse than the changes related to inflammation.
What about stage 4 CKD?
“Stage 4 kidney disease is a later stage of kidney disease. Patients in this stage are usually referred to a nephrologist and will likely be discussing the probability of dialysis or renal transplantation in the future. Patients with Stage 4 CKD often also have heart disease and other conditions. That is because the same root causes of CKD are lifestyle choices (lack of exercise, poor diets, high stress, smoking) that also contribute to heart disease and other conditions.
“If you have a large amount of inflammation, high blood pressure and high blood sugar, and only moderate scarring, when you adopt Ornish Lifestyle Medicine and address the root cause of the problem, your kidneys will get better. There are many reasons why Ornish Lifestyle Medicine works.” He continues to list a few of these:
- plant protein is easier on the kidneys than animal protein (ideally, this means opting for a WFPB diet)
- exercise is helpful for people with all stages of CKD
- social support is important in CKD (for instance, organised group support)
- stress management helps to improve health
The combined changes in your health can help to heal the kidneys as well as the heart. These include:
- lowering blood pressure
- decreasing blood sugar
- losing weight
- decreasing inflammation
- improving symptoms of depression
- . Together, these changes all help to heal changes to the kidneys as well as the heart.
“We routinely see participants with stage 1-3 CKD (And often with stage IV CKD) who are following the four elements of Ornish Lifestyle Medicine, improve their conditions in as short as nine weeks. Though this is common, it is not universal in stage IV. Some cases take longer, and in others, there is just too much scarring to reverse the disease or a different set of root causes for it.”
Dr Brown also recommends a low salt diet (which is naturally achieved through eating whole plant foods with no added salt). He also says it’s worth considering probiotics, and anti-inflammatory herbs such as curcumin (in turmeric) and boswellia.
They will also likely recommend a low salt diet. There may be additional benefits of a pure vegan diet, meaning no egg whites or dairy. And other supplements worth considering are probiotics, and anti-inflammatory herbs including curcumin and boswellia 19 .
Joe’s comments
I have no experience of boswellia, but do know that there are huge benefits in taking turmeric on a daily basis, as covered in detail by an earlier blog 20 . If you have certain types of kidney stones, it was recommended in the Part 2 2 that you should consider avoiding turmeric, although, as indicated, there’s some uncertainty about whether this is actually necessary in general cases of CKD.
The consensus from all the medical sources we’ve looked at in Parts 1-3 of this short series is that animal foods and processed foods should be avoided. The issue of potassium and phosphorus content is something that I think is still somewhat unresolved. There doesn’t appear to be sufficient research data on the effects of consuming naturally-occurring potassium and phosphorus in plant foods when the only foods consumed at whole plant foods – without the added salt, oils and sugar within the processed or home-prepared foods that we unfortunately see in many vegan diets.
In his book “Whole” 21 Dr T Colin Campbell stresses the incredible complexity of the billions of rapid interactions that take place within the human body. It would, therefore, seem rational to assume that testing the effects of individual foods on a person’s health might produce somewhat different results if the subject was eating the standard Western highly processed, animal-based diet as opposed to a WFPB diet without any added salt, oil or sugar. We’ll have to wait for the research data to appear in order to draw ultimate conclusions on this matter…
References
- Kidney Disease & WFPB Part 1 [↩]
- Kidney Disease & WFPB Part 2 [↩] [↩]
- Ornish Lifestyle Medicine Program [↩]
- Dr Dean Ornish: Research Highlights [↩]
- Ornish Living: Improving Chronic Kidney Disease with a Plant-Based Lifestyle
by Carra Richling [↩] - Carra Richling and the rest of the Ornish team [↩]
- Am J Kidney Dis. 2016 Mar;67(3):423-30. doi: 10.1053/j.ajkd.2015.10.018. Epub 2015 Dec 10. The Associations of Plant Protein Intake With All-Cause Mortality in CKD. Chen X, Wei G, Jalili T, Metos J, Giri A, Cho ME, Boucher R, Greene T, Beddhu S. [↩]
- WebMD: What Meds Might Hurt My Kidneys? [↩]
- Calcium and Phosphate Homeostasis. Joseph L Shaker, MD and Leonard Deftos, M.D. [↩]
- Clin J Am Soc Nephrol. 2011 Feb;6(2):257-64. doi: 10.2215/CJN.05040610. Epub 2010 Dec 23.
Vegetarian compared with meat dietary protein source and phosphorus homeostasis in chronic kidney disease.
Moe SM1, Zidehsarai MP, Chambers MA, Jackman LA, Radcliffe JS, Trevino LL, Donahue SE, Asplin JR. [↩] - Clin J Am Soc Nephrol. 2010 May; 5(5): 836–843. Associations of Diet with Albuminuria and Kidney Function Decline. Julie Lin, Frank B. Hu, and Gary C. Curhan [↩]
- Dtsch Arztebl Int. 2012 Jan;109(4):49-55. doi: 10.3238/arztebl.2012.0049. Epub 2012 Jan 27.
Phosphate additives in food–a health risk. Ritz E1, Hahn K, Ketteler M, Kuhlmann MK, Mann J. [↩] - How to Get Flavour Without Adding Salt [↩]
- Spice It Up: It’s Good For You!
by Carra Richling [↩] - High Potassium Fruits and Veg [↩]
- Low Potassium Fruits and Veg [↩]
- United States Department of Agriculture. Agricultural Research Service. USDA Food Composition Databases [↩]
- Ornish Living Magazine. I was Diagnosed with Stage 4 Chronic Kidney Disease. Can Ornish Lifestyle Medicine Help Control CKD? by Ben Brown, MD [↩]
- Wikipedia: Boswellia. [↩]
- Turmeric Proven To Fight Cancer & Diabetes [↩]
- Whole: Rethinking the Science of Nutrition by Dr T Colin Campbell and Howard Jacobson [↩]

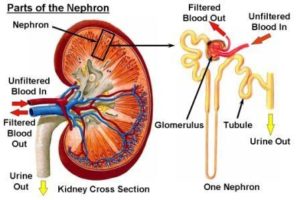 When all this excess protein is eliminated, the blood flow and filtration rates of the kidney tissues (called nephrons) increase, which in turn, causes a condition known as “intra-glomerular hypertension.”
When all this excess protein is eliminated, the blood flow and filtration rates of the kidney tissues (called nephrons) increase, which in turn, causes a condition known as “intra-glomerular hypertension.” 