
A previous blog 1 looked at a pre-published study on vitamin B12 status in Spanish vegetarians and vegans. Because there are very few reports on plant-based dietary patterns in Spain, this blog will look at the same study 2 in more detail, now that it has been published in its final form. While looking at B12 status amongst lacto-ovo vegetarians (LOV) and vegans (VN), it became clear that establishing true levels of this vitamin is a much more complex matter than most people realise. And, since side-effects of B12 deficiency are so nasty, this might be a blog worth reading – especially if you’re a plant-eater.
Thus, before looking at this study, it’s worth going into a bit more detail about vitamin B12.
Why is B12 status so important?
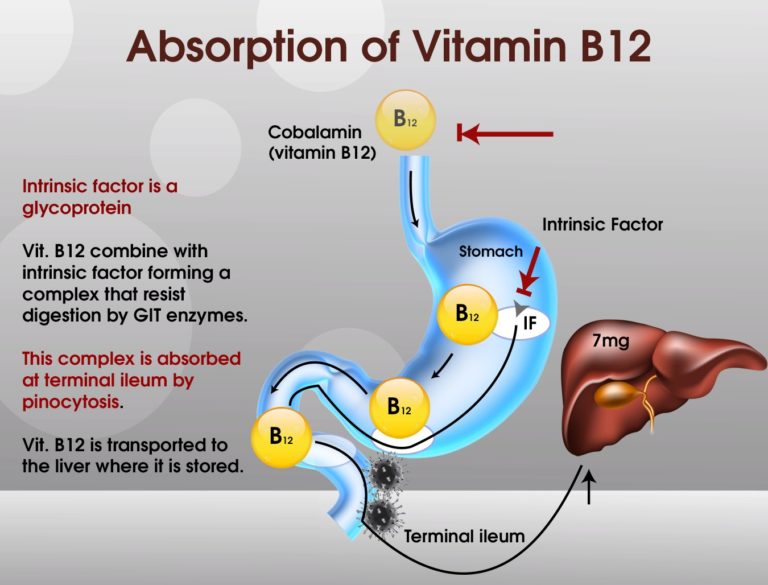
In normal healthy bodies, vitamin B12 (cobalamin) is readily absorbed in the distal ileum (the last part of the small intestine). However, in order for it to be absorbed, it must combine with a vital substance called intrinsic factor, which is a glycoprotein secreted by parietal cells of the gastric mucosa within the stomach. Without intrinsic factor, vitamin B12 will simply pass through the body and get excreted in stools.
Both vitamin B12 and vitamin B9 (folate) are necessary for the formation and maturation of red blood cells (erythrocytes) and the synthesis of DNA – the genetic material of cells. Vitamin B12 is also necessary for normal nerve function.
Since B12 is so essential for the formation of mature blood cells, any deficiency of this vitamin can result in anaemia, causing the body’s cells to receive insufficient oxygen from the haemoglobin within the red blood cells.
There are actually two forms of anaemia related to B12 deficiency and both are referred to as macrocytic anaemias 3 which can be either megaloblastic or pernicious anaemia:
Megaloblastic anaemia
This is characterised by abnormally large red blood cells (macrocytes) and abnormal white blood cells. It may not develop until 3-5 years after the deficiency starts. This is because around 3-5 years worth of B12 can be stored in the liver – so long as you’re an adult who has already been able to store sufficient quantities. No other B vitamin (or vitamin C) can be stored in the body like this, since they are all water-soluble (including B12) and are generally flushed out of the body if there is excess within the diet. On the other hand, the fat-based vitamins (A, E, D and K) can be stored in fat tissues as well as the liver. This means that daily intakes of the water-based vitamins (vitamins C, B1, B2, B3, B5, B6, B7, B9 and B12) is really important for maintenance of optimal health.
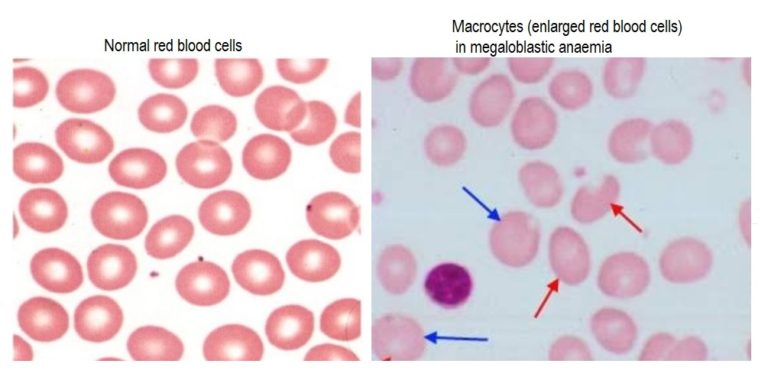
Megaloblastic anaemia is where insufficient B12 (or folate) is available to allow the normal DNA synthesis of red blood cells. It can be due to a number of causes, including:
- insufficient B12 in the diet
- overgrowth of bacteria in part of the small intestine
- impaired absorption (malabsorption disorders such as coeliac disease or certain pancreatic disorders)
- inflammatory bowel disease (IBD)
- fish tapeworm infection
- AIDS
- surgery that removes the part of the small intestine where vitamin B12 is absorbed
- drugs such as antacids and metformin (used to treat diabetes)
- repeated exposure to nitrous oxide (laughing gas)
- lack of intrinsic factor (see pernicious anaemia below)
- decreased stomach acidity (common among older people)
As we age, our ability to absorb B12 decreases. This happens irrespective of dietary habits, but obviously there’s a bigger threat of deficiency (in all ages) for those who don’t eat animal products- the major source of B12. Bacteria in the soil and elsewhere produce B12. Animals don’t actually produce it themselves. If we still drank from pure streams and ate food we picked up from untreated soils, we’d get sufficient B12. However, with chlorinated water, pesticide-treated soils, and shrink-wrapped food, we either have to eat animal products or take supplements to ensure we get enough B12. There are plants that contain some of the vitamin (see below), but they are generally considered insufficient on their own to maintain healthy B12 levels.
Pernicious anaemia
Pernicious anaemia is a form of megaloblastic anemia where intrinsic factor is lacking. There may well be plenty of B12 in the diet, but if intrinsic factor is not present or, for some other reason, is not able to play its role in the the absorption of vitamin B12 from the small intestine into the bloodstream, then the B12 passes through and out of the body. This may be due to a number of reasons. For instance, abnormal antibodies, produced by an overactive immune system, may attack and destroy the parietal cells in the stomach that produce intrinsic factor, resulting in an autoimmune reaction called autoimmune metaplastic atrophic gastritis. Alternatively, intrinsic factor may be lacking because the part of the stomach where intrinsic factor is produced has been surgically removed.
Symptoms of B12 deficiency
Anaemia caused by vitamin B12 deficiency develops gradually. This allows the body to adapt to some extent, but this can mean that symptoms are mild while the anaemia is actually very severe.
Mild anemia symptoms can include:
- paleness
- weakness
- fatigue
More serious anaemia symptoms can include:
- shortness of breath
- dizziness
- rapid heart rate
- spleen and liver enlargement
Pernicious anaemia in younger adults (due to lack of intrinsic factor) is more likely to result in the development of stomach and other gastrointestinal cancers.
B12 deficiency and nerve damage
Because B12 plays a significant role in the synthesis and maintenance of myelin4 , prolonged deficiency can result in damage to the central (CNS) and peripheral (PNS) nervous systems. In relation to CNS damage, white matter of the spinal cord and brain can suffer, resulting in such conditions as subacute combined degeneration (SCD) 5 and optic nerve atrophy. PNS issues are commonly manifested as nerve damage to the legs and arms, with the legs usually being affected earlier and more often than the arms. Symptoms include:
- tingling in the feet and hands
- loss of sensation in the legs, feet, and hands
- weakness in arms and legs
- loss of position sense – that is, people can’t tell so well where their arms and legs are and fail to feel vibrations
- mild to moderate muscle weakness
- loss of normal reflexes
- difficulty in walking
In addition to the above neurological effects, some people can also become confused, irritable, and mildly depressed.
Advanced vitamin B12 deficiency may lead to delirium, paranoia and impaired mental function, including dementia.
Diagnosis of B12 deficiency
Diagnosis is via:
- blood tests
- the Schilling test (often in younger patients)
- endoscopy
Blood tests
Routine serum blood tests can often show a suspected B12 deficiency if large red blood cells are detected. Since folate (vitamin B9) is also responsible for red blood cell synthesis, a possible B9 deficiency would normally also be investigated.
B12 deficiency can also be suspected if people complain of the typical symptoms associated with nerve damage, such as tingling or loss of sensation. If the deficiency is suspected, the level of vitamin B12 in the blood is measured.
Additionally, serum gastrin 6 levels or autoantibodies 7 to intrinsic factor may be measured.
Schilling test
The Schilling test involves the patient being given two doses of B12. The first is ‘labelled’ with a small amount of a radioactive substance and is then taken by mouth. The second is an injection one hour later of a larger amount of B12 that is not radioactively labelled, which is used in order to prevent any of the labelled B12 from binding to B12-depleted tissues.
After the injection is given, the amount of labelled B12 (that which had been taken orally) is measured by testing the urine to determine whether the body absorbed a normal (digested, rather than injected) amount of the vitamin.
If this normal amount has not been absorbed (revealed by a high amount being found in the urine), then the deficiency is confirmed. The same test is then repeated. This time, people are given intrinsic factor with the B12 taken by mouth. If intrinsic factor enables the body to absorb more of the vitamin, then it’s confirmed that the deficiency is caused by a lack of intrinsic factor, and the diagnosis of pernicious anemia can be made. If the B12 is still not absorbed, further tests are undertaken to check for potential problems with pancreatic enzymes or bacterial abnormalities.
More detail on this test can be found here 8 .
Endoscopy
Endoscopy is the use of a flexible viewing tube to directly examine internal structures. It may be done to check for destruction of the parietal stomach cells that produce intrinsic factor.
If vitamin B12 deficiency is confirmed in an older person, it’s unlikely that either Schilling or endoscopy will be used. This is because the cause is likely to be the usual age-related reduction in stomach acidity, and is usually not serious. However, in a younger person, other tests, including other blood tests, Schilling test and endoscopy are likely to be used in order to establish intrinsic factor status.
Folate, B12 deficiency & plant-based diets
It’s important to note that high folate (vitamin B9) levels can give a false negative for B12 deficiency. That is, high levels of folate in the blood sample can make it look like there’s no B12 deficiency. This is because the constant supply of folate allows the red blood cells to appear normal in size, while the other serious neurological damage of B12 deficiency can go unnoticed, in spite of the person having regular blood tests for B12 deficiency.
Of course, those people most likely to have a B12 deficiency while having high dietary folate intake are those eating a plant-based diet – given that there’s so much folate in plant foods. This is why B12 supplementation is so important.
Treatments for B12 deficiency
For less advanced deficiency, B12 supplements generally do the trick; however, if people already have nerve damage, or they have pernicious anaemia (for instance, caused by having had the part of the stomach removed which produced intrinsic factor), then the B12 is normally given by injections into a muscle for defined periods so long as the disorder is uncorrected.
Since the B12 in supplements is easier to absorb than that in meat, older people with deficiency can benefit from taking B12 supplements.
In most people with mild to moderate anaemia, there is a normalisation in around 6 weeks of treatment with high doses of B12 supplements. However, in severe cases due to nerve damage or loss of ability to produce intrinsic factor, the treatment by B12 injection could last for the rest of their lives.
Unfortunately, in those with dementia resulting from B12 deficiency (mostly older people), mental function would not be expected to improve after treatment.
How much B12 should I supplement?
I covered this subject in some detail in a previous blog 9 , which I suggest you take a look at if you are unsure about how often and how much B12 you should be supplementing.
Non-animal foods containing vitamin B12
Several mushroom species contain some B12, including:
- shiitake (Lentinula edodes)
- black trumpet (Craterellus cornucopioides), and
- golden chanterelle (Cantharellus cibarius)
Certain algae and cyanobacteria 10 such as:
The above are some of the foods normally used to produce B12 supplements for veggies and vegans.
Animal foods containing B12
Animal sources highest in vitamin B12 include meats (especially beef, pork, liver, and other organ meats), eggs, fortified cereals, milk, clams, oysters, salmon, and tuna.
It’s been reported that B12 deficiency exists much more widely in omnivore populations than one might imagine, since modern animal rearing practices are causing a reduction in the levels of B12 in meat. This can be seen particularly clearly, for instance, in the need to given cobalt supplements to cattle and sheep because of the reduced levels of cobalt in modern cultivated soils (B12 is called cobalamin because it contains a cobalt atom) 13 .
The Spanish study 2
The 49 lacto-ovo vegetarians and 54 vegans in the study filled out a Food Frequency Questionnaire (FFQ), and were tested to establish the following classical and functional markers (explanation of all terms in green can be seen by holding the cursor over the adjacent footnote number):
In broad terms, two parts of this study are of particular interest: firstly, the difficulties involved in accurately diagnosing B12 deficiency (and the suggested additional tests by which this can be more accurately diagnosed) and, secondly, to see if there was any pattern of B12 deficiency between the two groups – lacto-ovo-vegetarian (LOV) and vegan (VN).
1. Difficulties in diagnosing B12 deficiency
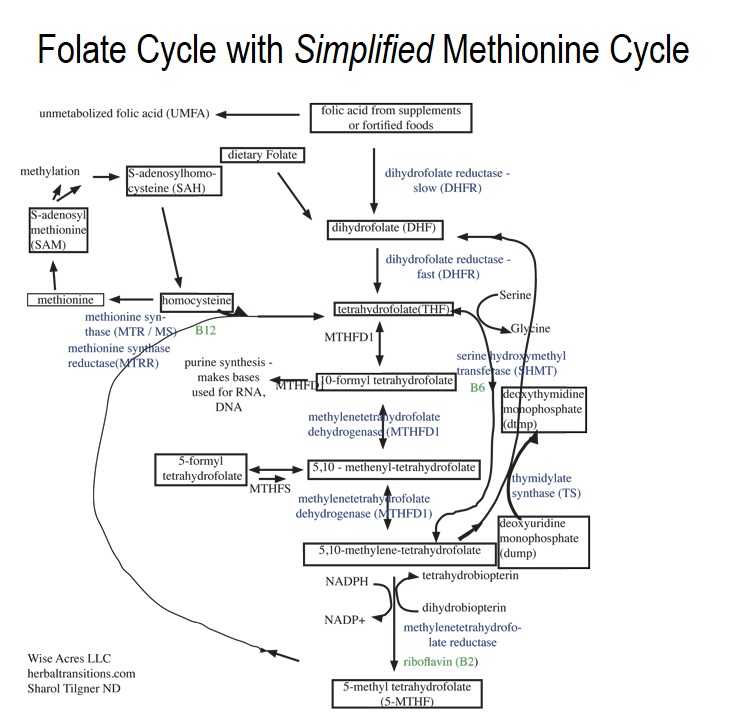
In order to understand the potential difficulties involved in diagnosing B12 deficiency, it’s useful to understand the vital processes B12 undergoes within the body, and this will involve knowing about two biological cycles: the methionine cycle and the folate cycle, both of which are essential for DNA and RNA synthesis, the production of red blood cells (erythropoiesis) and the production of neurotransmitters. 21 22
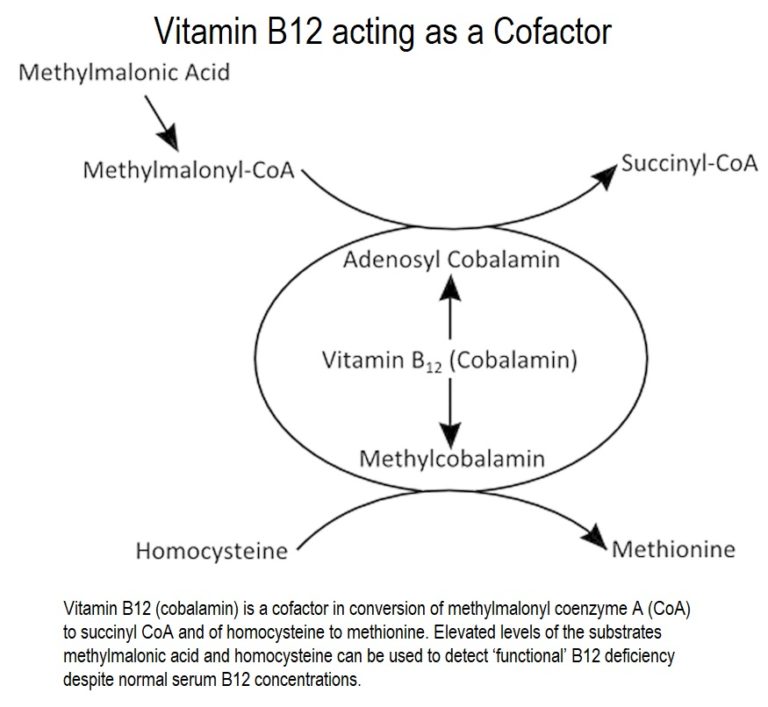 Vitamin B12 acts as a cofactor 23 of the enzymes methionine synthase 24 , which acts in the conversion of homocysteine (Hcy) to methionine, and methylmalonyl-CoA mutase 25 , that produces succinyl-CoA from methylmalonyl-CoA, the active form of methylmalonic acid (MMA)18 .
Vitamin B12 acts as a cofactor 23 of the enzymes methionine synthase 24 , which acts in the conversion of homocysteine (Hcy) to methionine, and methylmalonyl-CoA mutase 25 , that produces succinyl-CoA from methylmalonyl-CoA, the active form of methylmalonic acid (MMA)18 .
The above reactions are involved in the methionine cycle 26 and the folate cycle 27 , both essential for DNA and RNA synthesis, erythropoiesis and the production of neurotransmitters.
The folate cycle is so important to the methionine cycle (also called the methylation cycle) that it’s often included in descriptions and diagrams of the methionine cycle. The following diagram should give you an idea of how interlinked and complex these cycles are.
Problems with Serum B12 tests
As mentioned above, testing levels of serum B12 is probably the most widely used means of assessing deficiency. However, a major problem is that it can appear perfectly normal whilst, at the same time. functional deficiency still lurks unseen beneath the surface. The long latency period of B12 deficiency showing up in the blood serum can regularly produce both false positives and false negatives – that is, appearing to have a deficiency but not having one, or not appearing to have a deficiency but actually having one. 28
Folate (vitamin B9) & B12
Since it’s known both that high levels of folate can mask B12 deficiency and that low levels of folate can account for hyperhomocysteinaemia (HHcy)17 , it follows that testing for folate levels would be rather useful. By establishing that folate levels are high (as they are likely to be in most plant-eaters – unless, of course, they’re living on a diet of doughnuts and chips!) , it would be possible to quickly discard folate deficiency as being responsible for HHcy or the presence of megaloblastic anaemia. 29
Homocysteine & B12
Testing for homocysteine (Hcy) levels – a more specific marker of functional vitamin B12 deficiency – would be a useful additional test. This is because Hcy levels rise in the presence of cellular B12 deficiency. So, is that sorted, then? Well, not quite. Another problem arises – namely, that Hcy levels can also be raised with deficiencies of vitamins B9 (folate) or B6 (pyridoxine) as well as by diets rich in methionine 30 . So back to the drawing board.
Methylmalonic acid (MMA) & B12
So, what about testing for MMA levels? This represents probably the most specific marker for vitamin B12 deficiency, since it’s independent of folate and vitamin B6 status. MMA levels increase when there’s a B12 deficiency, and this happens even before there are any obvious clinical symptoms of the deficiency.
The more the merrier
So, the researchers in this study suggest that when testing for B12 deficiency, relying on just one single standard marker of deficiency is to be avoided. Instead, several markers should be used – levels of serum B12/B9, Hcy and MMA 31 .
2. B12 status of Spanish lacto-ovo-vegetarians & vegans
Finally, we come to the findings of this study:
- the overall prevalence of clinical vitamin B12 deficiency was very low in the individuals tested
- when serum B12 levels alone were tested, there was no indication of B12 deficiency in either diet group
Various B12 markers
However, when MMA was measured, some subclinical deficiencies were detected, particularly in the non-users of vitamin B12 supplements, with no significant differences between VN and LOV. With elevated MMA being detected in more than 10 % of the study subjects, it’s clear that using this marker to detect subclinical deficiencies is a pretty good idea.
- although macrocytosis (enlarged red blood cells) was observed in several participants, no clear relationship to any biomarkers of vitamin B12 deficiency could be found
- HHcy was found in more than 30 % of the subjects
They recommend that both MMA and Hcy (together with serum B12) should be used since each of these biomarkers gives information about the actions of B12 in different metabolic pathways. For instance, the metabolic reactions leading to the production of MMA and Hcy require different cobalamin forms:
- methylcobalamin acts in the Hcy pathway
- adenosylcobalamin acts in the formation of succinyl-CoA
The latter occur in different cell compartments:
- the methionine and folate cycles occur in the cell’s cytoplasm 32
- the synthesis of succinyl-CoA (SCS) 33 occurs in the mitochondria34
When B12 status was assessed with serum vitamin B12, MMA and Hcy simultaneously, the proportion of subjects with values out of range of at least one of the biomarkers was remarkably higher than the proportion detected by using only serum B12.
Most of the hyperhomocysteinaemic individuals presented mild HHcy (16–30 µmol/l) while only three volunteers had moderate HHcy (31–100 µmol/l).
Hcy variation in veggies from different European countries
Interestingly, this study comments on the fact that there’s great variability in the B12 values obtained in vegetarians from different European countries:
In the current study, Hcy was higher in LOV than in VN, which contrasted with other studies 37 .
High folate levels
Erythrocyte folate levels were high in all participants, with more than 50 % surpassing the suggested 38 cut-off for high erythrocyte folate (1360 nmol/l). This is in line with other research 39 that found higher folate intakes in plant-eaters than in omnivores.
Methionine & Hcy/HHcy
With folate repletion and under similar B12 levels, it was observed that LOV had higher levels of both Hcy and HHcy than VN. The researchers said this might be due to the fact that LOV consume more protein and, thus, more methionine, being that both dairy and egg are higher in methionine than plant foods. By increasing blood levels of Hcy, high methionine levels are linked to increased risk of heart disease, tumour growth, brain damage and even death.
The importance of supplementation
Various studies 37 have reported lower B12 levels in vegans, but this was not observed in the present study. The reason for this is thought to be that the members of both Spanish groups had a high and extended use of cobalamin (B12) supplements, with B12 supplement users exhibiting higher serum B12 and erythrocyte folate levels (as well as lower MMA and Hcy) than non-users. This underlines the importance of supplementation for vegans and lacto-ovo vegetarians.
These results are, of course, consistent with previous studies that recommend intake of B12 in supplement form. The reason generally given – which seems perfectly fair – is that it’s difficult for plant-eaters to achieve consistent and sufficient B12 levels without taking B12 supplements. The intake of fortified food items is not enough, of itself, to provide the required doses of the vitamin.40 41
Supplementation, diet or socioeconomic variation?
In recent studies on vegetarian Indians 42 43 , a prevalence of B12 deficiency was found in around 70 % of those tested, with more than 50 % of the subjects also presenting HHcy.
An explanation for this variation between results from Spain and India may be explained by differences in both diet composition and socioeconomic status. 44
However, even in studies of B12 status in European countries (where one would expect vegetarians to have similar socioeconomic status and diet composition as found in Spain), similar differences (that is, less B12 deficiency in Spanish vegetarians) was seen in Germany, the Netherlands and the UK. 45
Thus, the researchers maintain that the sufficient B12 status observed in both Spanish groups (LOV and VN) can be mainly accounted for by the extended use of cobalamin supplements in the Spanish participants compared with the lower amount of such supplementation reported in other European studies.
Spanish plant milks are not fortified
Having spent a significant time at our mountain retreat in Spain, it has always interested me that the Spanish do not fortify their plant milks – unlike the UK and elsewhere in Europe. This is a very good reason why any veggie living (or spending extended periods) in Spain should not rely on plant milks for their B12. Indeed, the current study emphasises that such milks had no influence on the analysed biomarkers in this research, being that these milks are not B12-fortified.
Final thoughts
Two limitations of this study were, firstly, that they didn’t add an additional omnivore group for comparison, since this would have shown whether and by how much these groups (LOV and VN) differed from the general meat-eating Spanish population and, secondly, this was a small sample (103 individuals) from which to generalise to the whole Spanish LOV and VN population – of which veggies are thought 46 to comprise around 1.5%.
What would have been interesting, in addition, would have been to include a WFPB dietary group. Naturally, this is something that would prove very difficult in almost any country (perhaps excluding certain ‘enlightened’ populations within the US), since the number of people eating a WFPB diet is still very low.
The report did not consider the influence of any potential genetic polymorphisms 47 that might be involved in the B12 and folate routes. Perhaps future B12 studies could look at this, as well as include a larger number of subjects and include both omnivores and those eating a WFPB diet.
In any case, the take-home message is that anyone eating a plant-based diet needs to take B12 supplementation. It’s a cheap and highly effective way of avoiding health conditions that would undo some of the wonderful work achieved by eating this way.
References & Notes
- B12 Supplements Are Efficient But Caution With Folic Acid [↩]
- J Nutr Sci. 2019 Feb 26;8:e7. doi: 10.1017/jns.2019.2. eCollection 2019. Vitamin B12 and folate status in Spanish lacto-ovo vegetarians and vegans. Gallego-Narbón A, Zapatera B, Barrios L, Vaquero MP. [↩] [↩]
- The term macrocytic is from Greek words meaning “large cell”. A macrocytic class of anaemia is an anaemia (defined as blood with an insufficient concentration of haemoglobin) in which the red blood cells (erythrocytes) are larger than their normal volume. [↩]
- Myelin is an insulating layer, or sheath that forms around nerves, including those in the brain and spinal cord. It is made up of protein and fatty substances. This myelin sheath allows electrical impulses to transmit quickly and efficiently along the nerve cells. [↩]
- Subacute combined degeneration (SCD) is characterised by symmetric dysesthesia, disturbance of position sense and spastic paraparesis or tetraparesis. [↩]
- Gastrin is a hormone which stimulates secretion of gastric juice and is secreted into the bloodstream by the stomach wall in response to the presence of food. [↩]
- An autoantibody is antibody produced by in response to a constituent of its own tissues. [↩]
- Schilling Test Kamleshun Ramphul; Stephanie G. Mejias. Statpearls. [↩]
- Vegan Society Veg-1: Does It Contain Enough B12? [↩]
- Cyanobacteria are a division of microorganisms related to bacteria but which are capable of photosynthesis. They are prokaryotic and represent the earliest known form of life on the earth. [↩]
- a genus of single-celled green algae belonging to the division Chlorophyta. [↩]
- Spirulina is a biomass of cyanobacteria (blue-green algae) from the two species Arthrospira platensis and A. maxima. It can be consumed by humans and other animals. Arthrospira is cultivated worldwide and is used as a dietary supplement or whole food, being also used as a feed supplement in the aquaculture, aquarium, and poultry industries. [↩]
- J Dairy Sci. 1979 Aug;62(8):1195-206. Trace element deficiencies and fertility in ruminants: a review. Hidiroglou M. [↩]
- In blood, serum is the liquid part but without the clotting factors (mainly fibrinogens). The liquid part with the clotting factors is the plasma. Serum still includes all the other proteins not used in blood clotting, along with all the electrolytes, antibodies, antigens, hormones, and any exogenous substances. [↩]
- Red blood cell (erythrocyte) folate concentrations respond slowly to changes in dietary folate intake since the erythrocytes, which have a 120-day lifespan, accumulate folate only during the production of new red blood cells (erythropoiesis). Red blood cell folate concentrations are useful as indicators of long-term folate status. [↩]
- Homocysteine (an intermediate in the metabolism of the amino acids methionine and cysteine) is a common amino acid in your blood. You get it mostly from eating meat. High levels of it are linked to early development of heart disease. and is associated with low levels of vitamins B6, B12, and folate, as well as with renal disease. [↩]
- Hyperhomocysteinaemia is a medical condition characterised by an abnormally high level of homocysteine in the blood, conventionally described as being above 15 µmol/L. Hyperhomocysteinaemia is typically managed with vitamin B6, vitamin B9 and vitamin B12 supplementation. Hyperhomocysteinaemia promotes the formation of active oxygen species and the release of inflammatory mediators, and therefore it is considered a risk factor for cardiovascular disease (CVD). [↩] [↩]
- Methylmalonic acid (MMA) is a substance produced in very small amounts and is necessary for human metabolism and energy production. The measurement of elevated amounts of methylmalonic acid in the blood or urine serves as a sensitive and early indicator of vitamin B12 deficiency. [↩] [↩]
- Mean corpuscular haemoglobin is the average mass of haemoglobin per red blood cell in a sample of blood. High MCH levels are commonly a sign of the macrocytic anaemia seen in B12 or folate deficiency. [↩]
- Mean corpuscular volume is a measure of the average volume of a red blood corpuscle. The measure is attained by multiplying a volume of blood by the proportion of blood that is cellular, and dividing that product by the number of erythrocytes in that volume. High MCV implies the red blood cells are larger than normal (i.e. macrocytic) and is a test of B12 and folate deficiency. [↩]
- Krishnaswamy K & Madhavan Nair K (2001) Importance of folate in human nutrition. Br J Nutr 85, Suppl. 2, S115–S124. [↩]
- Kapoor A, Baig M, Tunio SA, et al. (2017) Neuropsychiatric and neurological problems among vitamin B12 deficient young vegetarians. Neurosciences (Riyadh) 22, 228–232. [↩]
- A cofactor is a non-protein chemical compound or metallic ion that is required for an enzyme’s activity. Cofactors can be considered “helper molecules” that assist in biochemical transformations. [↩]
- Methionine is an essential amino acid that has to be derived from our diet. Methionine synthase is responsible for the regeneration of methionine from homocysteine. [↩]
- Methylmalonyl-CoA mutase (MCM) is a protein that in humans is encoded by the MUT gene. This vitamin B12-dependent enzyme catalyses the isomerisation of methylmalonyl-CoA to succinyl-CoA in humans. [↩]
- In the methionine cycle, methionine (a sulphur-containing amino acid which enters the body through dietary proteins) is used in forming proteins in the body. In the methionine cycle, methionine acts as the precursor of the sulphur-containing amino acids homocysteine, cysteine, and taurine. Taurine is one of the few amino acids not used in protein synthesis, and is thus usually referred to as a “nonessential” amino acid, or more generously as a “conditionally essential” amino acid. [↩]
- Within the folate cycle, folate coenzymes are responsible for the one-carbon unit transfer in intermediary metabolism and are required for several reactions in key metabolic processes, for example of purine, pyrimidine and methionine synthesis, and glycine and serine metabolism. [↩]
- Klee GG (2000) Cobalamin and folate evaluation: measurement of methylmalonic acid and homocysteine vs vitamin B12 and folate. Clin Chem 46, 1277–1283. [↩]
- Krajcovicova-Kudlackova M, Blazicek P, Kopcova J, et al. (2000) Homocysteine levels in vegetarians versus omnivores. Ann Nutr Metab 44, 135–138. [↩]
- Kumar A, Palfrey HA, Pathak R, et al. (2017) The metabolism and significance of homocysteine in nutrition and health. Nutr Metab (Lond) 14, 78. [↩]
- Yetley EA, Pfeiffer CM, Phinney KW, et al. (2011) Biomarkers of vitamin B12 status in NHANES: a roundtable summary. Am J Clin Nutr 94, 313S–321S. [↩]
- Cytoplasm is a thick solution that fills each cell and is enclosed by the cell membrane. It’s mainly composed of water, salts, and proteins. All the organelles, such as the nucleus, endoplasmic reticulum, and mitochondria, are located in the cytoplasm within eukaryotic cells. Organelles are the organised or specialised structures within a living cell. Eukaryotic cells are cells that contain a nucleus and organelles, enclosed by a plasma membrane. Humans are composed of eukaryotic cells and are thus grouped into the biological domain Eukaryota. Eukaryotic cells are larger and more complex than prokaryotic cells, which are found in Archaea and Bacteria, the other two domains of life. [↩]
- Succinyl-CoA or SCS facilitates the flux of molecules into other metabolic pathways by controlling the interconversion between succinyl CoA and succinate. This is important because succinyl CoA is an intermediate necessary for porphyrin, haem, and ketone body biosynthesis. It’s a necessary part of the energy-producing Krebs or citric acid cycle. [↩]
- The mitochondria is an organelle found in large numbers in most cells, in which the biochemical processes of respiration and energy production occur – the “powerhouses” of energy production. [↩]
- Waldmann A, Koschizke JW, Leitzmann C, et al. (2004) Homocysteine and cobalamin status in German vegans. Public Health Nutr 7, 467–472. [↩]
- Majchrzak D, Singer I, Manner M, et al. (2006) B-vitamin status and concentrations of homocysteine in Austrian omnivores, vegetarians and vegans. Ann Nutr Metab 50, 485–491. [↩]
- Elmadfa I & Singer I (2009) Vitamin B12 and homocysteine status among vegetarians: a global perspective. Am J Clin Nutr 89, 1693S–1698S. [↩] [↩]
- Colapinto CK, O’Connor DL & Tremblay MS (2011) Folate status of the population in the Canadian Health Measures Survey. CMAJ 183, E100–E106. [↩]
- Schüpbach R, Wegmüller R, Berguerand C, et al. (2017) Micronutrient status and intake in omnivores, vegetarians and vegans in Switzerland. Eur J Nutr 56, 283–293. [↩]
- Gilsing AM, Crowe FL, Lloyd-Wright Z, et al. (2010) Serum concentrations of vitamin B12 and folate in British male omnivores, vegetarians and vegans: results from a cross-sectional analysis of the EPIC-Oxford cohort study. Eur J Clin Nutr 64, 933–939. [↩]
- Pawlak R, Lester SE & Babatunde T (2014) The prevalence of cobalamin deficiency among vegetarians assessed by serum vitamin B12: a review of literature. Eur J Clin Nutr 68, 541–548. [↩]
- Naik S, Mahalle N & Bhide V (2018) Identification of vitamin B12 deficiency in vegetarian Indians. Br J Nutr 119, 629–635. [↩]
- Yajnik CS, Deshpande SS, Lubree HG, et al. (2006) Vitamin B12 deficiency and hyperhomocysteinemia in rural and urban Indians. J Assoc Physicians India 54, 775–782. [↩]
- Menal-Puey S & Marques-Lopes I (2017) Development of a food guide for the vegetarians of Spain. J Acad Nutr Diet 117, 1509–1516. [↩]
- Herrmann W, Schorr H, Obeid R, et al. (2003) Vitamin B12 status, particularly holotranscobalamin II and methylmalonic acid concentrations, and hyperhomocysteinemia in vegetarians. Am J Clin Nutr 78, 131–136. [↩]
- AECOSAN (2011) National Survey of Dietary Intake (2009–2010). Results on Consumption Data. Madrid: Spanish Agency for Consumer Affairs, Food Safety and Nutrition Government of Spain. [↩]
- Polymorphisms are the occurrence of different forms among the members of a population or colony, or in the life cycle of an individual organism. [↩]

