
In the last blog 1 we looked at Dr McDougall’s views on diet and kidney disease. This blog will look at what Dr Michael Greger 2 has to say on this important subject.

As we look at the advice Dr Greger gives, we will also dig a little deeper into some recent research studies that complement and expand his observations.
Dr Greger – How not to die from kidney disease
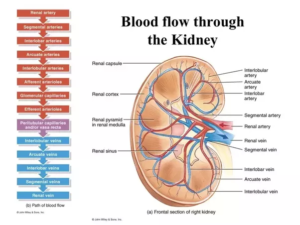
In a 2016 video 3 on this specific topic, Dr Greger explains that it’s perfectly rational to expect a plant-based diet can not only prevent but also treat kidney failure. This is because kidneys are highly vascular organs, and we know that blood vessels throughout the body can be clogged up and impaired by eating the wrong diet. But what is the “wrong” diet?
A 2010 Harvard study 4 looked at how diet influences microalbuminuria 5 and estimated GFR (eGFR) 6 decline in people with well-preserved kidney function. They found that there were three significant dietary risk factors for loss of kidney function:
- animal protein
- animal fat
- cholesterol
The researchers conclude: that “Higher dietary intake of animal fat and two or more servings per week of red meat may increase risk for microalbuminuria. Lower sodium and higher beta-carotene intake may reduce risk for eGFR decline.”
Another earlier study 7 explained how animal fat literally clogs up vessels inside the kidney. The following photos of autopsied kidneys show just how badly clogged up they can get,

A 1998 study 8 showed how animal protein can kick the health out of normal kidney function, leading to hyperfiltration, where the kidneys have to work too hard and eventually can fail completely.
But what about plant protein?
A 1989 study 9 showed clearly that animal protein, even good old tuna fish, can increase pressure on the kidneys within a hours of eating your so-called ‘healthy’ tuna sandwich – and this applies to both non-diabetics and diabetics. The researcher concluded: “Plasma concentrations of alanine, glycine, and arginine [amino acids derived from the animal protein], known to induce glomerular hyperfiltration, increased to a greater degree after ingestion of tuna fish meal than after administration of bean curd. These findings suggest that responses of GFR to acute protein loading may differ according to the amino acid composition of the protein ingested and to the stage of diabetic nephropathy.” And as Dr Greger says: “…we’re not talking adverse effects decades down the road, but literally within hours of it going into our mouth.” 3
The following is a chart from the latter study, showing clearly that tuna protein and soy protein have profoundly different effects on the kidneys.

The composition of amino acids within proteins, and the subtle but important differences between amino acids composition in animal vs plant proteins, are fascinating subjects, and nobody is better qualified to talk about them than Dr T Colin Campbell 10 .
Dr Greger raises no concerns about plant protein being a causal factor in declining kidney function. Indeed he states clearly: “Dealing with plant protein is no problem.” 3
What’s mechanism is involved?
Inflammation is triggered when you eat animal products, and this inflammation causes the kidney overload. We’ve already looked at this in some detail in a previous blog 11 , and it’s a phenomenon already demonstrated in earlier studies, one of which 12 demonstrated that the animal protein caused the inflammation. They achieved this by looking at the inflammatory responses in subjects when they consumed animal products alone, and then when they consumed them with a powerful anti-inflammatory drug. In the former case, there was an inflammatory response; in the latter, none.
So, simple choice: eat your animal products in combination with a powerful anti-inflammatory drug, or eat a plant-based diet.
Then there’s the acid load…
Again, we’ve already looked 13 at the issue of acidity in animal-based diets, but it’s worth re-emphasising that animal protein induces acid formation in the kidneys. A 2014 study 14 demonstrated that animal foods (all meat, eggs, and dairy) cause acid to form within the kidneys and this may then lead to an unpleasant condition called tubular toxicity (damage to the tiny, delicate, urine-making tubes in the kidney). This, in turn, may lead to ATN (acute tubular necrosis) where the tubular epithelial cells that form the renal tubules of the kidneys die. The researchers conclude that: “The findings have important implications, in that, if they are corroborated in other studies, altering diets may provide an adjunct approach to other strategies for treatment of CKD [chronic kidney disease].”
And, indeed, other studies 15 16 have corroborated their findings.
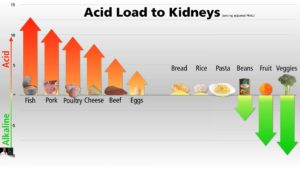
Which animal food is most acid-forming?
You may be surprised to hear that Dr Greger considers fish the worst offender, followed by pork and poultry. Plant foods, of course, are somewhere between neutral and alkaline. A useful chart from his video 3 gives a little more detail:
A 2012 study 17 suggests that the key to slowing or stopping the progression of chronic kidney disease is more likely to be found in a grocery store, than in a pharmacy.
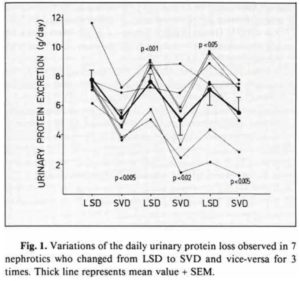
Dr Greger points out that plant-based diets have been used to treat kidney disease for decades. He cites a 1990 study 18 which did an interesting experiment. They took subjects who had declining kidney function and put them on alternating diets – the first, a typical low-sodium diet (LSD) that doctors put CKD patients on and, the second, a standard vegan diet (SVD) to test the protein leakage from the kidneys. The following chart shows that simply changing the diet will turn off or on kidney dysfunction like a light switch:
An additional article 19 on nutritionfacts.org (Dr Greger’s website) makes some other interesting points:
- to maintain kidney health, avoid the following:
- toxic metal contamination
- NeuG5c 20
- alpha-gal 21
- advanced glycation end products (AGEs) 22
- meat (including poultry and processed meat)
- other animal proteins
- sugar
- salt
- high-fat meals
- chewing betel nuts 23
- star fruit 24 25
- possibly chamomile tea – since nutritionfacts states that its safety for those with CKD has not yet been established. Interestingly, other authorities consider it positively beneficial for those with CKD 26
- high-temperature cooking may create kidney cancer causing carcinogens 27
- if you have certain kidney stones, the author on nutritionfacts.org recommends that one should avoid nutritional yeast, turmeric, and beets [I find this one a bit odd since I haven’t yet found research to show that nutritional yeast impairs kidney function; I have found research 28 that actually supports turmeric for improved kidney health; beets, on the other hand, are high in potassium and, as mentioned in Part 1 29 , may well be good to limit in the late stages of CKD.]
- to maintain kidney health, include the following:
- stay well hydrated (drink at least ten cups of water per day)
- consume phytates (found in beans, nuts, seeds, and grains) to reduce kidney stone risk
- eat a plant-based diet
The article concludes: “Overall, plant-based diets appear to boost kidney health. Plant-based, fiber-rich diets may protect against kidney and other cancers, reduce the risk of childhood prediabetes (which can lead to kidney damage) and diabetes, the top cause of kidney failure. No surprise, then, that plant-based diets can be used to both help prevent and treat kidney failure.” 19
In another more recent 2018 article 30 , Dr Greger expounds on the importance of avoiding an acid-forming diet in order to maintain kidney health:
“Acid-inducing diets are believed to affect the kidney through tubular toxicity, damage to the tiny, delicate, urine-making tubes in the kidney via increased ammonia production. Ammonia is a base, so the kidney creates 31 it to buffer the acid from the food we eat. This is beneficial in the short term to get rid of the acid; however, in the long term, all that extra ammonia in our kidneys day in and day out seems to exert toxic effects.
Our kidney function tends to decline 32 progressively after our 30s, and, by our 80s, our kidney capacity may be down to half. “Perhaps, the so-called age-related decline in renal function is a result of damage induced 33 by ammonia overproduction.” That’s just one theory, though. The acidic pH may increase the production of free radicals and damage the kidney that way, or add to scarring.
Not only is protein derived from plant foods accompanied by antioxidants 34 that can fight the free radicals, but plant protein is 35 also less acid-forming in the first place because it tends to have fewer sulfur-containing amino acids. One of the reasons plant foods tend to be less acid-forming than animal foods is because acid is produced 36 by the sulfur in the protein, and there’s less in plant proteins.”
In Part 3, we’ll look at the thoughts of Dr Dean Ornish’s medical/research team at his Preventive Medicine Research Institute (PMRI).
Joe’s comments
Most of what Dr Greger says is in line with Dr McDougall’s recommendations. Once again, it appears that the take-home message is that a whole food plant-based diet (with no added salt, oil or sugar) is the ideal option for those who want to prevent or do their best to halt the progression of kidney disease.
References
- Kidney Disease & WFPB Part 1 [↩]
- Dr Michael Greger’s website [↩]
- How Not to Die from Kidney Disease. Michael Greger M.D. FACLM October 12th, 2016 Volume 32 [↩] [↩] [↩] [↩]
- Lin J, Hu FB, Curhan GC. Associations of diet with albuminuria and kidney function decline. Clin J Am Soc Nephrol. 2010 May;5(5):836-43. [↩]
- Definition of microalbuminuria: a term to describe a moderate increase in the level of urine albumin. It occurs when the kidney leaks small amounts of albumin into the urine, in other words, when there is an abnormally high permeability for albumin in the glomerulus of the kidney. [↩]
- Definition of eGFR: an abbreviation for estimated glomerular filtration rate. Your eGFR is a number based on your blood test for creatinine, a waste product in your blood. It tells how well your kidneys are working. [↩]
- Hartroft WS. Fat emboli in glomerular capillaries of choline-deficient rats and of patients with diabetic glomerulosclerosis. Am J Pathol. 1955 May-Jun;31(3):381-97. [↩]
- Soroka N, Silverberg DS, Greemland M, Birk Y, Blum M, Peer G, Iaina A. Comparison of a vegetable-based (soya) and an animal-based low-protein diet in predialysis chronic renal failure patients. Nephron. 1998;79(2):173-80. [↩]
- Nakamura H, Takasawa M, Kashara S, Tsuda A, Momotsu T, Ito S, Shibata A. Effects of acute protein loads of different sources on renal function of patients with diabetic nephropathy. Tohoku J Exp Med. 1989 Oct;159(2):153-62. [↩]
- Animal vs. Plant Protein. October 29, 2013. By T. Colin Campbell, PhD [↩]
- Animal Foods Are The Smoking Gun [↩]
- Trevisan R, Valerio A, Avogaro A, Borsato M, Doria A, Semplicini A, Sacerdoti D, Jones S, Bognetti E, et al. Impaired renal response to a meat meal in insulin-dependent diabetes: role of glucagon and prostaglandins. Am J Physiol. 1990 Mar;258(3 Pt 2):F675-83. [↩]
- Alkaline Diet – So What?! [↩]
- Banerjee T, Crews DC, Wesson DE, Tilea A, Saran R, Rios Burrows N, Williams DE, Powe NR; Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team. Dietary acid load and chronic kidney disease among adults in the United States. BMC Nephrol. 2014 Aug 24;15:137. [↩]
- Nutrients. 2017 Apr; 9(4): 374. Published online 2017 Apr 10. Vegetarian Diet in Chronic Kidney Disease—A Friend or Foe. Anna Gluba-Brzózka, Beata Franczyk, and Jacek Rysz. [↩]
- National Kidney Association: Plant Protein Reduces Mortality in Chronic Kidney Disease Patients [↩]
- Uribarri J, Oh MS. The key to halting progression of CKD might be in the produce market, not in the pharmacy. Kidney Int. 2012 Jan;81(1):7-9. [↩]
- Barsotti G, Cupisti A, Morelli E, Ciardella F, Giovannetti S. Vegan supplemented diet in nephrotic syndrome. Nephrol Dial Transplant. 1990;5 Suppl 1:75-7. [↩]
- Kidney Disease: nutritionfacts.org article [↩] [↩]
- Definition of NeuG5c: N-Glycolylneuraminic acid is a sialic acid molecule found in most non-human mammals. Humans cannot synthesize Neu5Gc because the human gene CMAH is irreversibly mutated, though it is found in apes. [↩]
- Definition of alpha-gal: Galactose-alpha-1,3-galactose (alpha-gal) is a carbohydrate found in the cells of many mammals that humans eat, such as cows, sheep, and pigs. … People with this allergy may experience mild discomfort after eating meat, or they may have a dangerous reaction that leaves them unable to breathe. Alpha-gal syndrome is a recently identified type of food allergy to red meat. [↩]
- Definition of AGEs: Advanced glycation end products (AGEs) are proteins or lipids that become glycated as a result of exposure to sugars. They can be a factor in aging and in the development or worsening of many degenerative diseases, such as diabetes, atherosclerosis, chronic kidney disease, and Alzheimer’s disease. [↩]
- Public Health Nutr. 2009 May;12(5):723-7. doi: 10.1017/S1368980008003339. Epub 2008 Jul 23. Association between betel-nut chewing and chronic kidney disease in men. Chou CY, Cheng SY, Liu JH, Cheng WC, Kang IM, Tseng YH, Shih CM, Chen W. [↩]
- BMC Res Notes. 2015; 8: 796. Star fruit toxicity: a cause of both acute kidney injury and chronic kidney disease: a report of two cases. R. A. Abeysekera,corresponding author S. Wijetunge, N. Nanayakkara, A. W. M. Wazil, N. V. I. Ratnatunga, T. Jayalath, and A. Medagama. [↩]
- National Kidney Foundation: A TO Z HEALTH GUIDE. Why You Should Avoid Eating Starfruit. [↩]
- CKD Website: Can You Drink Chamomile Tea If You Have Renal Failure [↩]
- Science Daily: Increased meat consumption, especially when cooked at high temperatures, linked to elevated kidney cancer risk [↩]
- Molecules. 2014 Dec 2;19(12):20139-56. doi: 10.3390/molecules191220139. Curcumin and chronic kidney disease (CKD): major mode of action through stimulating endogenous intestinal alkaline phosphatase. Ghosh SS1, Gehr TW2, Ghosh S3. [↩]
- High potassium vegetables [↩]
- Reduce Acid-Forming Proteins to Protect Kidney Function. Written By Michael Greger M.D. FACLM on July 24th, 2018 [↩]
- J Nephrol. 2011 Jan-Feb;24(1):11-7. Dietary acid load and rapid progression to end-stage renal disease of diabetic nephropathy in Westernized South Asian people. van den Berg E1, Hospers FA, Navis G, Engberink MF, Brink EJ, Geleijnse JM, van Baak MA, Gans RO, Bakker SJ. [↩]
- N Engl J Med. 1982 Sep 9;307(11):652-9. Dietary protein intake and the progressive nature of kidney disease: the role of hemodynamically mediated glomerular injury in the pathogenesis of progressive glomerular sclerosis in aging, renal ablation, and intrinsic renal disease. Brenner BM, Meyer TW, Hostetter TH. [↩]
- Am J Nephrol. 2014;39(2):142-4. doi: 10.1159/000358602. Epub 2014 Feb 7. Is dietary Acid a modifiable risk factor for nephropathy progression? Goraya N1, Wesson DE. [↩]
- Am J Kidney Dis. Author manuscript; Am J Kidney Dis. 2013 Aug; 62(2): 267–275. Lifestyle-Related Factors, Obesity, and Incident Microalbuminuria: The CARDIA (Coronary Artery Risk Development in Young Adults) Study. Alex Chang, Linda Van Horn, David R. Jacobs, Jr., Kiang Liu, Paul Muntner, Britt Newsome, David Shoham, Ramon Durazo-Arvizu, Kirsten Bibbins-Domingo, Jared Reis, and Holly Kramer. [↩]
- Clin J Am Soc Nephrol. 2011 Jul; 6(7): 1526–1532. Estimated Net Endogenous Acid Production and Serum Bicarbonate in African Americans with Chronic Kidney Disease. Julia J. Scialla, Lawrence J. Appel,Brad C. Astor, Edgar R. Miller, III, Srinivasan Beddhu,§Mark Woodward, Rulan S. Parekh, and Cheryl A.M. Anderson [↩]
- Am J Nephrol. 2014;39(2):145-52. doi: 10.1159/000358262. Epub 2014 Feb 11. Dietary acid intake and kidney disease progression in the elderly. Kanda E, Ai M, Kuriyama R, Yoshida M, Shiigai T. [↩]

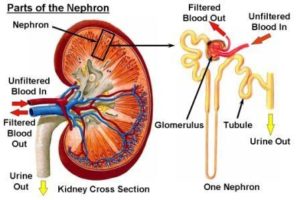 When all this excess protein is eliminated, the blood flow and filtration rates of the kidney tissues (called nephrons) increase, which in turn, causes a condition known as “intra-glomerular hypertension.”
When all this excess protein is eliminated, the blood flow and filtration rates of the kidney tissues (called nephrons) increase, which in turn, causes a condition known as “intra-glomerular hypertension.” 