Animal protein vs plant protein. Lectins in uncooked beans vs salmonella in uncooked poultry. What’s the point of changing your diet? They’re all just as bad as each other. I think not! If you look through the research studies on the relationship between diet and chronic illnesses, such as diabetes, obesity, cardiovascular disease, cancer etc, you will see a consistent pattern: animal foods (meat, eggs, fish and dairy) are associated with increased risk and plant foods (fruit, veg, legumes, nuts and seeds) are associated with decreased risk. Animal foods appear to be the smoking gun – time after time. This blog looks a quick overview of just a bit of the evidence. And where there’s a smoking gun pointed at the corpse, who fired the shot?
I suggest it wasn’t the boiled broccoli but the fried beef. Does the research bear this out?
Blog Contents
Where’s the beef? Look for the inflammation.
When you look at illness and disease you can quite reasonably start with the causes of inflammation. Inflammation is the smoking gun. Wherever you find foods that cause inflammation (which comes as a boot up the backside of your immune system to switch up a gear – not a good thing, unless you have a cut or break, and certainly not a good thing as a background reality day by day, year by year because of the delicious morsels you pile into your body)1 . If you are sucking tobacco smoke into lungs on a daily basis, you will get inflammation. It slows down and eventually stops when you ditch the ciggies. The same thing appears to happen when you cut out the meat, eggs and cheese.2
Dr John McDougall knows from experience
As Dr McDougall says: “Research does not support the theory that carbohydrates from wheat, other grains, or starchy vegetables are the source of injury that leads to chronic inflammation. In contrast, scientific research does solidly support that the source of injury leading to chronic inflammation is animal foods.”3
So what causes inflammation – animal or plant foods?
Best way of dealing with this one is by giving you some research data.
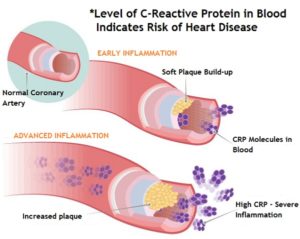 A European Journal of Nutrition (EJN) article entitled “Consumption of Red Meat and Whole-Grain Bread in Relation to Biomarkers of Obesity, Inflammation, Glucose Metabolism, and Oxidative Stress.”4 concludes: “The results of this study suggest that high consumption of whole-grain bread is related to lower levels of GGT5 , ALT6 , and hs-CRP7 , whereas high consumption of red meat is associated with higher circulating levels of GGT and hs-CRP.
A European Journal of Nutrition (EJN) article entitled “Consumption of Red Meat and Whole-Grain Bread in Relation to Biomarkers of Obesity, Inflammation, Glucose Metabolism, and Oxidative Stress.”4 concludes: “The results of this study suggest that high consumption of whole-grain bread is related to lower levels of GGT5 , ALT6 , and hs-CRP7 , whereas high consumption of red meat is associated with higher circulating levels of GGT and hs-CRP.
A 2013 review8 entitled “Dietary Pattern Analysis and Biomarkers of Low-Grade Inflammation: a Systematic Literature Review” drew the conclusion: “…biomarkers of inflammation were almost all meat-based or due to “Western” eating patterns.”
A 2014 American Journal of Clinical Nutrition article9 concluded: “Greater red meat intake is associated with unfavorable plasma concentrations of inflammatory and glucose metabolic biomarkers in diabetes-free women.”
So what about grains – do they inflame like meat?
Of course they don’t. But here’s some of the research data.
A 2010 Journal of Nutrition article10 concluded that women who consumed a serving or more a day of whole grains had a lower probability of having moderate or elevated hs-CRP7 , according to the AHA (American Heart Association) criteria, compared with non-consumers.
A 2012 Nutrition Reviews article11 concluded: “Epidemiological studies provide reasonable support for an association between diets high in whole grains and lower C-reactive protein (CRP) concentrations. After adjusting for other dietary factors, each serving of whole grains is estimated to reduce CRP concentrations by approximately 7%.”
And last, but but only in the very limited list of research covered, a 2013 Nutrition Journal article12 concluded: “Diets high in whole grains are associated with a 20-30% reduction in risk of developing type-2 diabetes… biomarkers of systemic inflammation tend to be reduced in people consuming high intakes of whole grains.”
The smoking gun is always meat, not plants. I know that this is a pain in the rump steak of most meat-eaters, but it appears to be facts-based.
I will leave you with a meta-analysis from the Journal of Nutrition13 which concluded that those consuming grains (rather than meat) had a 26% reduction in the risk of type-2 diabetes and a 21% reduction in the risk of heart disease (independent of known CVD risk factors). Furthermore, there is an inverse relationship between whole grain intake and weight gain. That is, eat your whole grains and you will lose unnecessary/unhealthy (fatty) weight. Examples of whole grains included whole wheat, dark bread, oats, brown rice, rye, barley, and bulgur.
So where does this leave us?
It’s always a question of facts or, perhaps better said, the preponderance of facts (in a media-controlled technological world), and you can decide for yourself, admittedly based on my rather arbitrary-selected range of studies, who is holding the smoking gun – Colin the Cabbage or Peter the Port chop?

References
- Cell. 2010 Mar 19;140(6):871-82. doi: 10.1016/j.cell.2010.02.029. Nonresolving inflammation. Nathan C1, Ding A. [↩]
- JAMA. 1998 Dec 16;280(23):2001-7. Intensive lifestyle changes for reversal of coronary heart disease. Ornish D1, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ. [↩]
- The Smoke and Mirrors behind Wheat Belly and Grain Brain by Dr John McDougall. [↩]
- Eur J Nutr. 2013 Feb;52(1):337-45. doi: 10.1007/s00394-012-0340-6. Epub 2012 Mar 18. Consumption of red meat and whole-grain bread in relation to biomarkers of obesity, inflammation, glucose metabolism and oxidative stress. Montonen J, Boeing H, Fritsche A, Schleicher E, Joost HG, Schulze MB, Steffen A, Pischon T. [↩]
- Gamma-glutamyl transpeptidase (GGT) test. … GGT is concentrated in the liver, but it’s also present in the gallbladder, spleen, pancreas, and kidneys. GGT blood levels are usually high when the liver is damaged. This test is often done with other tests that measure liver enzymes if there’s a possibility of liver damage. [↩]
- ALT – alanine aminotransferase. While ALT is useful as an initial test in detecting liver disease, emerging data highlight its potential value as a measure of overall health and survival. There is a strong relationship between ALT activity and mortality, even when the life‐threatening process does not originate from the liver. [↩]
- C-reactive protein (CRP) is a protein that the liver makes when there is inflammation in the body. It’s also called a marker of inflammation, and can be measured with an hs-CRP (high-sensitivity C-reactive protein) test, sometimes also called a CRP test. … Excessive inflammation has been linked to heart disease. [↩] [↩]
- Nutr Rev. 2013 Aug;71(8):511-27. doi: 10.1111/nure.12035. Epub 2013 Jun 13. Dietary pattern analysis and biomarkers of low-grade inflammation: a systematic literature review. Barbaresko J1, Koch M, Schulze MB, Nöthlings U. [↩]
- Am J Clin Nutr. 2014 Feb;99(2):352-60. Associations between red meat intake and biomarkers of inflammation and glucose metabolism in women. Ley SH, Sun Q, Willett WC, Eliassen AH, Wu K, Pan A, Grodstein F, Hu FB. [↩]
- The Journal of Nutrition. Nutritional Epidemiology. Whole Grains Are Associated with Serum Concentrations of High Sensitivity C-Reactive Protein among Premenopausal Women. Audrey J. Gaskins, Sunni L. Mumford, Alisha J. Rovner, Cuilin Zhang, Liwei Chen, Jean Wactawski-Wende, Neil J. Perkins, and Enrique F. Schisterman, [↩]
- Nutr Rev. 2012 Jul;70(7):387-96. doi: 10.1111/j.1753-4887.2012.00487.x. Epub 2012 May 22. Effect of whole grains on markers of subclinical inflammation. Lefevre M, Jonnalagadda S. [↩]
- Belobrajdic and Bird Nutrition Journal 2013, 12:62. The potential role of phytochemicals in wholegrain cereals for the prevention of type-2 diabetes. Damien P Belobrajdic and Anthony R Bird. [↩]
- The Journal of Nutrition. Nutritional Epidemiology. Greater Whole-Grain Intake Is Associated with Lower Risk of Type 2 Diabetes, Cardiovascular Disease, and Weight Gain. Eva Qing Ye, Sara A. Chacko, Elizabeth L. Chou, Matthew Kugizaki, and Simin Liu. [↩]