I know from personal experience within my family that arthritis can be an excruciatingly painful disease which imposes significant limits on the quality of one’s life. At first inspection, it seems too good to be true that making simple dietary and lifestyle changes could significantly improve the symptoms of arthritis; but delving into the research (and eating the diet myself) has shown that it’s possible, not only to reduce arthritic pain, but to remove the major symptoms completely, allowing the body to heal itself where it can.
Blog Contents
What is Arthritis?
It’s really a group of diseases causing swollen and painful joints.
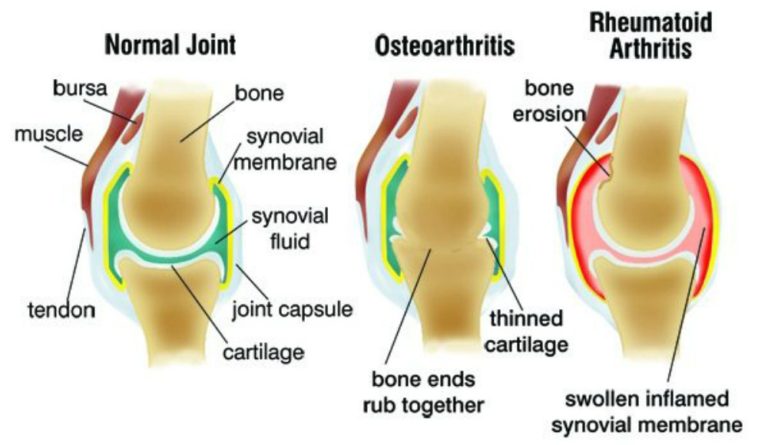
Osteoarthritis (OA) is usually a gradual degeneration of joint cartilage and underlying bone which is most common from middle age onward – indeed, OA is “the most frequent cause of physical disability among older adults” in the world 1 . It results in stiffness and pain, especially in the hip, knee, and thumb joints. It’s commonly thought that OA is merely unavoidable wear and tear, but this is not the case. In fact, it’s an active joint disease with a prominent inflammatory component.
Rheumatoid arthritis (RA) is where the body itself attacks the joints in a much more aggressive manner. As a chronic progressive disease, the inflammation it causes in the joints can result in painful deformity and immobility, especially in the fingers, wrists, feet, and ankles.
Genes & Arthritis
There are genetic predispositions within families, making it more or less likely that a person may develop RA. However, just because there’s a genetic predisposition, it does not necessarily mean that those genes have to be triggered and, hence, dictate the course of events in a person’s life.
Inflammation & Arthritis
We’ve already looked 2 at how the foods we eat can significantly affect the inflammation within our bodies. There is strong evidence that dietary changes can help to prevent the development of arthritis and, if it has already developed, to reduce inflammation and, thereby, potentially to eliminate the pain and stiffness altogether. Basically, get rid of the foods that spark the inflammatory responses within the joints, and you get rid of the inflammation.
“A survey of more than 1,000 arthritis patients revealed that red meat, sugar, fat, salt, caffeine, and nightshade plants (e.g., tomatoes, eggplant) most commonly worsen the condition. Research also shows that dairy protein may make symptoms worse.” 3
Research on Diet & Osteoarthritis
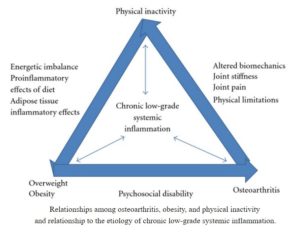
A 2012 study 4 considered that dietary changes along with increased physical exercise represents the best first-line option in preventing and treating OA: “Healthy living can be exploited to reduce inflammation, oxidative stress, and related pain and disability and improve patients’ overall health. This approach aligns with evidence-based best practice and holds the promise of eliminating or reducing chronic low-grade inflammation, attenuating disease progression, reducing weight, maximizing health by minimizing a patient’s risk or manifestations of other lifestyle-related conditions hallmarked by chronic low-grade inflammation, and reducing the need for medications and surgery. This approach provides an informed cost effective basis for prevention, potential reversal, and management of signs and symptoms of chronic osteoarthritis.”
A 2015 study 5 considered whether people with OA could benefit from dietary changes. They found that those eating a WFPB diet were able to report a significant decrease in their OA pain – and this was in just 2 weeks. At the end of the six-week study, they also reported more energy and better physical functioning, too. The study concluded: “…results suggest that a whole-foods, plant-based diet significantly improves self-assessed measures of functional status among osteoarthritis patients.”
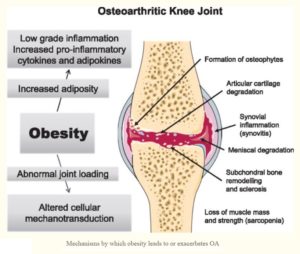
Osteoarthritis & Obesity
We’ve already looked at the powerful evidence 6 7 8 showing that the best, safest and most sustainable diet to prevent and treat obesity consists of moving away from all animal and processed food and replacing them with whole plant foods. But what about the relationship between OA and obesity?
A 2018 study 9 considered the evidence for a strong link between obesity and OA. It concluded: “With excess adiposity appearing to underlie the metabolic factors now recognized as being integral to OA, particularly of the hand and knee 10 11 , dietary modification to achieve weight reduction where appropriate, together with increased physical activity, are the strongest evidence-based recommendations.”
Obesity is a significant risk factor for developing OA. And it’s not just a matter of obesity putting more pressure on the joints. Within the joints, fatty tissue represents a potent source of pro-inflammatory chemicals that actively increase cartilage breakdown. When you lose weight, there are fewer of these chemicals and the symptoms of OA improve. It’s not rocket science to realise that the modern Western diet is going to supply the body with ample amounts of these pro-inflammatory chemicals which, in turn, will build up and put increased stress on joints.
Which Foods Fight Osteoarthritis?
Whilst I would always suggest that it’s best to focus on eating a varied and balanced plant diet, rather than merely focusing on the latest individual ‘miracle’ foods that regularly hit the media, there are some specific plant foods that research has indicated are particularly good for preventing and treating OA, including:
- turmeric curcumin 12
- ginger 13
- sesame seeds 14
- rose hips 15
- soy protein 16
- coriander/cilantro 17
- acai berries 18
- sulforaphane in broccoli/cabbage leaves 19
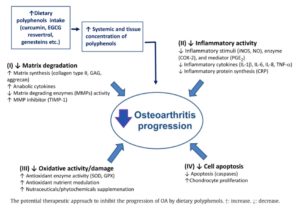
A 2012 study 20 looked at some of the mechanisms (particularly the molecular antiosteoarthritic mechanisms) involved in how OA may be prevented and treated by the polyphenols in common plant foods, including:
- turmeric curcumin
- epigallocatechin gallate 21 and green tea extract
- resveratrol 22
- nobiletin 23 and citrus fruits
- pomegranate
- genistein 24 and soy protein
Research on Diet & Rheumatoid Arthritis
It’s been known for some time that diet can have a notable affect on RA.
A 2000 study 25 looked at whether following a raw vegan diet rich in antioxidants and fibre could decrease joint stiffness and pain in patients with RA. The study stated: “In conclusion the rheumatoid patients subjectively benefited from the vegan diet rich in antioxidants, lactobacilli and fibre, and this was also seen in objective measures.”
A 2001 study 26 found a gluten-free, vegan diet was of significant benefit in improving the signs and symptoms of RA, with the authors concluding: “…this benefit may be related to a reduction in immunoreactivity to food antigens eliminated by the change in diet.”
A 2001 systematic review 27 concluded that fasting followed by a vegetarian or vegan diet might be useful in the treatment of RA: “The pooling of these studies showed a statistically and clinically significant beneficial long-term effect. Thus, available evidence suggests that fasting followed by vegetarian diets might be useful in the treatment of RA.”
A 2002 study 28 looked at the how a very low-fat vegan diet would affect individuals with moderate-to-severe RA. It only took 4 weeks on the diet to see significant improvements in the following:
- morning stiffness
- RA pain
- joint tenderness, and
- joint swelling
Which Foods Fight Rheumatoid Arthritis?
Whatever helps to prevent/treat OA would, you’d imagine, also help with RA. Again, picking out specific plants or phytochemicals is not the ideal approach, compared with simply eating a balanced and varied WFPB diet; but, as mentioned above, there are some specific foods which it’s worth pointing out have been shown as potentially helpful in preventing/treating RA, including:
- turmeric 29 30
- rosehip 31
- coriander/cilantro 32
- sour cherries & pomegranates 33
- ginger 34
- green tea 35
- parsley 36
Of course, an astonishingly wide range of inflammatory-fighting polyphenols are in all fruit and vegetables, and so any balanced WFPB diet will help to inhibit platelet activity which is associated with inflammation.
What Mechanisms Are Involved?
Things are changing in our view of arthritis. The question of just how central inflammation and immune responses are in the causation and prolongation of both OA and RA is an unfolding journey of discovery. It would appear to me as though the research is heading towards concluding that the role of immune responses and inflammation – and, hence, the primary role of diet in preventing both of these bodily reactions – is a lot more important in the pathogenesis of arthritis in general.
For instance, one study 37 comments: “Osteoarthritis (OA) has traditionally been classified as a noninflammatory arthritis; however, the dichotomy between inflammatory and degenerative arthritis is becoming less clear with the recognition of a plethora of ongoing immune processes within the OA joint and synovium.”

Naturally, if the joint defences (the cartilage) are chronically damaged, any excessive exercise or trauma to that joint will exacerbate joint damage; however, studies are revealing that it’s the food we eat, to some not-insignificant extent, that causes cartilage damage (or fails to protect the cartilage in the first place).
One study 38 looked at the role of WFPB diets in the treatment of OA, describing OA as: “...a group of mechanical abnormalities involving the degradation of articular cartilage and subchondral bone in the joints….A variety of causes including hereditary, developmental, metabolic, and mechanical etiologies may initiate the process of cartilage loss. As cartilage thins, bony surfaces become less well-protected and bone may be exposed or damaged. Regional muscles may experience atrophy and ligaments become more lax as a result of decreased movement secondary to pain.”
The same study concludes: “The present and earlier studies provide further evidence for the beneficial effects of WFPB diets in many patients with OA. We hope that the results from the current study will encourage an increased appreciation and clinical evaluation of dietary variables and that WFPB diet therapies are recommended as an adjunct to standard medical management of this debilitating chronic disease.”
In a podcast entitled “Healthy Joints” 39 , Dr Greger reinforces this by analysing how a plant-based diet protects our joints against arthritis. The common feature throughout, is the association between joint damage (be it via cartilage breakdown/loss of bone density or via autoimmune responses) and the consumption of animal foods.
In one of his short videos entitled “Preventing Arthritis”40 , Dr Greger draws a clear link between the pathogenesis of arthritis and the consumption of animal foods: “...eating meat—even a tiny amount—may dramatically increase our risk of developing degenerative arthritis. Even eating meat less than once a week may trigger arthritis. My patients will say things to me like, they only smoke x number of cigarettes, and my response is always that any amount of smoking is too much.”
Plenty of other research supports this view of the link between consuming animal foods and developing arthritis, with one study 41 concluding: “Greater meat consumption is associated with a higher prevalence of degenerative arthritis and soft tissue disorders in both male and female subjects of this population…”
Dr Greger on Arthritis & Animal Foods
Dr Greger mentions 42 one particular case: “…a case report of a woman eating eggs, dairy, and meat with joint inflammation so bad she was on chemo and steroids—until she stopped ingesting animal products, and her symptoms disappeared when she just ate plant proteins. She could turn on and off her disease like a light switch. It even says how she ate meat the night before her doctor’s appointment, just to show the doctor that she really did have bad arthritis…
“When susceptible people put all these foreign animal proteins in their body, one of two things may happen. When we nibble on the cartilage at the end of a chicken’s leg, our immune system may react to these foreign cartilage proteins by producing anti-cartilage antibodies that may get confused, and start attacking our own cartilage. That’s what they mean by meat-induced joint attack. The other possibility is that even if there are no cross-reactivity confusions, the immune complexes formed by the meat proteins and our antibodies may migrate into our joints and trigger inflammation that way.”
Animal Fats & Arthritis
Dr Neil Barnard posits 43 the possibility that animal fats may have a causal relationship with arthritis: “Plant-based diets are often lower in fat and contain different kinds of fat than diets with animal products. For example, many whole plant foods have an optimal ratio of omega-6 to omega-3 fats. Healthful weight loss from eating a vegan diet is also anti-inflammatory, further helping cool irritated joints.”
Dr Barnard goes on to provide two food lists – one that’s thought to help and the other that’s thought to exacerbate the symptoms of arthritis. He suggests that you eat an abundance of foods on the former list and avoid all foods on the latter list. Any foods that do not appear on either list, he suggests can be eaten freely. He also suggests that sufferers monitor if there are any foods that clearly trigger symptoms. These should be removed from the diet to see if their removal improves symptoms.
Foods That Help Alleviate Arthritis Symptoms
These ‘pain-safe foods’ virtually never contribute to arthritis, headaches, or other painful conditions:
- brown rice
- cooked green vegetables
- cooked orange vegetables
- cooked yellow vegetables
- cooked or dried non-citrus fruits
Common Trigger Foods To Be Avoided
- animals foods (this means all fish, meat, eggs and dairy)
- alcoholic beverages (especially red wine)
- monosodium glutamate (MSG)
- aspartame (NutraSweet)
Foods Reported As Potential Trigger Foods In Some Sufferers
- caffeinated drinks (coffee, tea, and colas)
- nitrites [Shown to be responsible in animal foods, but research 44 45 46 does not appear to support this in plant-foods.]
- chocolate [Research 47 48 seems to suggest this does not apply to plain unsweetened cocoa – it’s the usual sweetened dairy chocolate that’s the problem.]
- citrus Fruits [Some recent research 49 questions whether this is indeed the case, since there may be a protective aspect of citrus fruits for those with arthritis, particularly RA.]
- wheat [There’s uncertainty here about whether it’s the processed wheat in white bread and pastries that’s the issue. I suspect that wholegrains do not present the same potential to trigger arthritis symptoms, since other research 50 includes them in the anti-inflammatory diet suggested for arthritis sufferers.]
- nuts and peanuts [Alternative research 51 suggests that nuts and seeds are beneficial for arthritis sufferers.]
- tomatoes [Arthritis Research UK state 52 that they know of no research proving a link between tomatoes and arthritis. I guess this also relates to other nightshade veg.]
- onions [Other research 53 considers alliums (including onions, garlic and leeks) to be protective against arthritis.]
- corn [I’ve found no research that supports the notion that whole corn (either fresh on a cob or dried whole) has negative effects on arthritis. Once again, I suggest it’s when the corn is eaten as an isolated oil or within fast-food snacks that problems arise.]
- apples [This is an odd one, since research 54 55 indicates that apples are excellent for both reducing inflammation and providing a rich supply of easily-absorbed vitamin C and other phytonutrients.]
- bananas [Comments by Arthritis Research UK 56 exemplify the confusion over bananas and arthritis by saying that there’s anecdotal evidence both for and against bananas for relieving arthritis symptoms. As far as I can see, there’s no solid research evidence either way.]
My suspicion with some of the above ‘triggers’ is that they have become anecdotally associated with increasing arthritic symptoms rather than because there is any convincing research evidence.
Of course, this is not to claim that these foods cannot trigger arthritis symptoms in some people, but this appears to be the typical situation where people focus on one particular ‘bad boy’ food rather than their whole diet – often in the hope that, thereby, they won’t have to radicalise their diet and remove favourite food (meat, fast-food, snacks, confectionery, processed foods) to which they are virtually addicted and which they can’t imagine living without. More of this below in relation to wholism vs reductionism.
Joint Damage in Athletes
We looked previously 57 58 59 in some detail at how a plant-based diet protects athletes against joint and muscle damage, as well as being effective in helping to heal the body more quickly from exercise-related injury. Thus, it would make sense that making the right choice between a diet consisting of pro-inflammatory animal-foods or of anti-inflammatory plant-foods may be a primary factor in the pathogenesis and development of both OA and RA. This is made more probable when we take into account how plant-foods are shown 60 to provide such strong support for the body’s immune system, for instance through producing the ideal microbiome in our guts.
Gout – A Form of Arthritis
In a previous blog specifically on gout 61 , we looked in great detail at how the consumption of animal-foods is perhaps the major cause of this excruciating condition; conversely, we saw that transitioning to a wholefood plant-based diet (as well as making other lifestyle changes, such as cutting out alcohol) prevents and treats gout more effectively than current medications – and without all the associated side-effects of the latter.
Wholism vs Reductionism
Once again, it’s possible to pan out on this whole topic and conjecture that a more wholistic approach to disease prevention and treatment – one that would deal with the vast range of seemingly interlinked conditions, such as obesity, diabetes, heart-disease, hypertension, immune disease and inflammatory diseases – is the way to kill more than one disease with just one diet.
As discussed in a previous blog 62 , modern medicine appears to have fallen into a reductionist trap, where drug companies (and thereby medical practitioners) are on a constant race to find one specific drug to treat – what they think is – one specific disease. An alternative paradigm is that all medical conditions are linked in complex ways within our bodies and, since we are what we eat, the thing that most dramatically and directly affects this complex of bodily conditions is the food we put in our mouths.
Final Thoughts
Six of One or Half a Dozen of the Other
So, to some extent, the most important general questions might not be whether arthritis is caused by animal protein-induced autoimmune attack in the joints or by the animal proteins/fats themselves attacking the joints; rather, perhaps we should be stepping back and looking at the elephant in the room – the animal foods themselves. This is particularly the case when animal foods are eaten to excess in highly processed form, as is the norm within the Western diet.
Maybe Confusion is a Good Thing Sometimes
If the above has left you with a degree of confusion about which specific foods are good or bad for the prevention/treatment of different forms of arthritis, then maybe that’s not as bad a thing as it might at first appear.
After all, we only understand a small fraction of the incredibly complex interactions of the tens of thousands of nutrients in foods – and this is apart from our relative ignorance of the precise ways in which these interactions affect the tissues, organs, processes and trillions of interrelated cells within our bodies. In the above-mentioned blog, Wholism vs Reductionism 62 , this was well-demonstrated by looking at just one diagrammatic representation of the partial metabolic processes involved in one single cell:
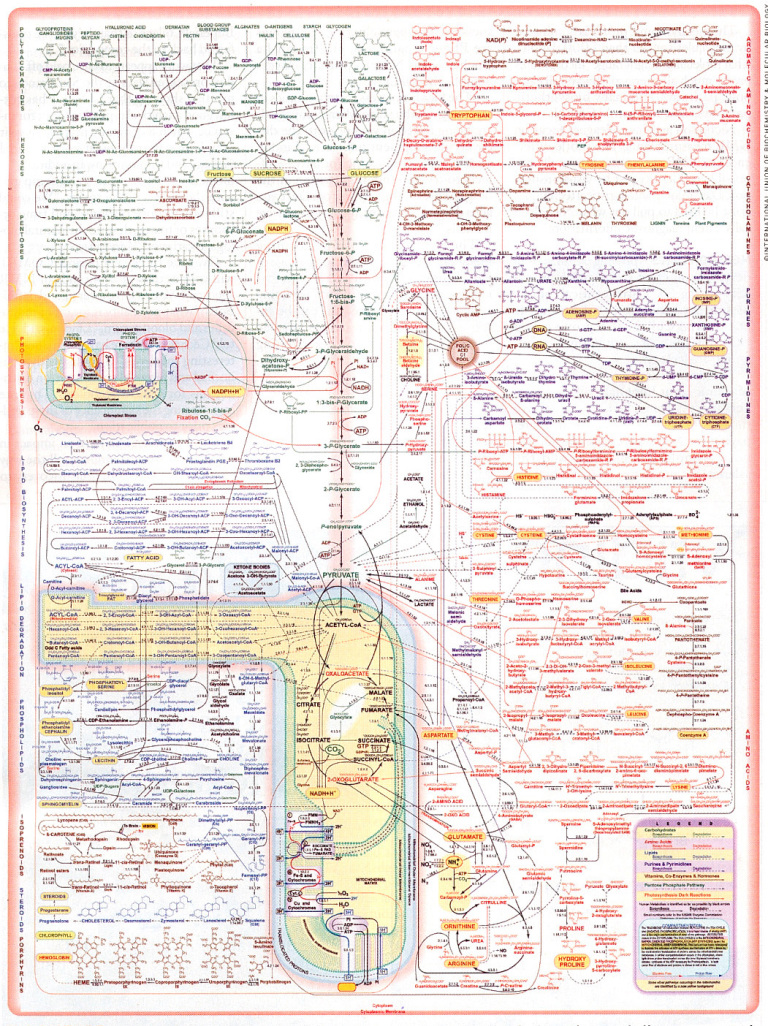
Don’t even try to read this, let alone understand it.
As Professor T Colin Campbell adds 63 :
“The fact that each nutrient passes through such a maze of reaction pathways suggests that each nutrient also is likely to participate in multiple health and disease outcomes. The one nutrient/one disease relationship implied by reductionism, although widely popular, is simply incorrect. Every nutrient-like chemical that enters this complex system of reactions creates a rippling effect that may extend far into the pool of metabolism. And with every bite of food we eat, there are tens and probably hundreds of thousands of food chemicals entering this metabolism pool more or less simultaneously.”
So, we’re faced with the same choice in terms of arthritis as we are with all the non-communicable diet-related diseases which are growing at terrifying rates within our populations: do we wait until the media, health authorities, politicians and food manufacturers/retailers own up to the reality of plant-based diets being the optimal choice for humans, or do we take our own health in our hands and choose the WFPB dietary route for ourselves today?
References
- T. Neogi, Y. Zhang. Epidemiology of osteoarthritis. Rheum. Dis. Clin. North Am. 2013 39(1):1 – 19. [↩]
- Depression is Linked to Inflammation [↩]
- Focus on plant-based foods to ease arthritis pain. [↩]
- E. Dean, R. G. Hansen. Prescribing optimal nutrition and physical activity as first-line interventions for best practice management of chronic low-grade inflammation associated with osteoarthritis: Evidence synthesis. Arthritis. 2012 2012:560634. [↩]
- Clinton CM, O’Brien S, Law J, Renier CM, Wendt MR. Whole-foods, plant-based diet alleviates the symptoms of osteoarthritis. Arthritis. 2015;2015:708152-708161. [↩]
- Want to Lose Weight the Easy Way? [↩]
- Can The UK Government Really Combat Child Obesity? [↩]
- England’s Obesity Hotspots [↩]
- Rheumatology – Oxford. 2018 May. What is the evidence for a role for diet and nutrition in osteoarthritis? Sally Thomas, Heather Browne, Ali Mobasheri, and Margaret P Rayman. [↩]
- Monira Hussain S, Wang Y, Cicuttini FM. et al. Incidence of total knee and hip replacement for osteoarthritis in relation to the metabolic syndrome and its components: a prospective cohort study. Semin Arthritis Rheum 2014;43:429–36. [↩]
- Visser AW, de Mutsert R, le Cessie S. et al. ; NEO Study Group. The relative contribution of mechanical stress and systemic processes in different types of osteoarthritis: the NEO study. Ann Rheum Dis 2015;74:1842–7. [↩]
- Turmeric Curcumin & Osteoarthritis. Michael Greger M.D. FACLM January 17th, 2014 Volume 16. [↩]
- Ginger for Osteoarthritis. Michael Greger M.D. FACLM December 5th, 2016 Volume 33 [↩]
- Sesame Seeds for Knee Osteoarthritis. Michael Greger M.D. FACLM November 7th, 2016 Volume 33 [↩]
- Rose Hips for Osteoarthritis. Michael Greger M.D. FACLM September 17th, 2010 Volume 4 [↩]
- Phytomedicine. 2004 Nov;11(7-8):567-75. Soy protein may alleviate osteoarthritis symptoms. Arjmandi BH, Khalil DA, Lucas EA, Smith BJ, Sinichi N, Hodges SB, Juma S, Munson ME, Payton ME, Tivis RD, Svanborg A. [↩]
- Antioxidant and antiarthritic potential of coriander (Coriandrum sativum L.) leaves. Article in e-SPEN Journal 7(6):e223–e228 · December 2012. [↩]
- The Science on Açaí Berries. Written By Michael Greger M.D. FACLM on August 22nd, 2013 [↩]
- Benefits of Cabbage Leaves on the Knee for Osteoarthritis. Michael Greger M.D. FACLM June 18th, 2018 Volume 42 [↩]
- C.-L. Shen, B. J. Smith, D.-F. Lo, M.-C. Chyu, D. M. Dunn, C.-H. Chen, I.-S. Kwun. Dietary polyphenols and mechanisms of osteoarthritis. J. Nutr. Biochem. 2012 23(11):1367 – 137. [↩]
- Wikipedia: Epigallocatechin gallate [↩]
- Wikipedia: Resveratrol [↩]
- Wikipedia: Nobiletin [↩]
- Wikipedia: Genistein [↩]
- Hänninen, Kaartinen K, Rauma AL, et al. Antioxidants in vegan diet and rheu-matic disorders. Toxicology. 2000;155:45-53 [↩]
- Hafström I, Ringertz B, Spångberg A, et al. A vegan diet free of gluten im-proves the signs and symptoms of rheumatoid arthritis: the effects on arthritis correlate with a reduction in antibodies to food antigens. Rheumatology (Ox-ford). 2001;40:1175-1179. [↩]
- Müller H, de Toledo FW, Resch KL. Fasting followed by vegetarian diet in patients with rheumatoid arthritis: a systematic review. Scand J Rheumatol.2001;30:1-10. [↩]
- McDougall J, Bruce B, Spiller G, Westerdahl J, McDougall M. Effects of a very low-fat, vegan diet in subjects with rheumatoid arthritis. J Altern Complement Med. 2002;8:71-75. [↩]
- Turmeric Curcumin & Rheumatoid Arthritis. Michael Greger M.D. FACLM January 15th, 2014 Volume 16 [↩]
- J Med Food. 2016 Aug;19(8). Efficacy of Turmeric Extracts and Curcumin for Alleviating the Symptoms of Joint Arthritis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Daily JW, Yang M, Park S. [↩]
- Aust Fam Physician. 2012 Jul;41(7):495-8. Rosehip – an evidence based herbal medicine for inflammation and arthritis. Cohen M. [↩]
- Toxicol Ind Health. 2014 Sep;30(8):738-49. Nutraceuticals of anti-inflammatory activity as complementary therapy for rheumatoid arthritis. Al-Okbi SY [↩]
- Adv Biomed Res. 2014; 3: 100. Potent health effects of pomegranate. Aida Zarfeshany, Sedigheh Asgary, Shaghayegh Haghjoo Javanmard. [↩]
- PharmaNutrition. 2016 Jul;4(3):123-131. Epub 2016 Jun 4. Anti-Inflammatory Effects of the Essential Oils of Ginger (Zingiber officinale Roscoe) in Experimental Rheumatoid Arthritis. Funk JL, Frye JB, Oyarzo JN, Chen J, Zhang H, Timmermann BN. [↩]
- Rheumatoid Arthritis. Regulation of Transforming Growth Factor β–Activated Kinase Activation by Epigallocatechin‐3‐Gallate in Rheumatoid Arthritis Synovial Fibroblasts: Suppression of K63‐Linked Autoubiquitination of Tumor Necrosis Factor Receptor–Associated Factor 6. Anil K. Singh Sadiq Umar Sharayah Riegsecker Mukesh Chourasia Salahuddin Ahmed. First published: 16 October 2015. [↩]
- Int J Mol Sci. 2016 Jun 9;17(6). Flavonoids as Cytokine Modulators: A Possible Therapy for Inflammation-Related Diseases. Leyva-López N, Gutierrez-Grijalva EP, Ambriz-Perez DL, Heredia JB. [↩]
- Ther Adv Musculoskelet Dis. 2013 Apr; 5(2): 77–94. Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Jeremy Sokolovecorresponding, Christin M. Lepus. [↩]
- Arthritis. Volume 2015, Article ID 708152, 9 pages. Clinical Study. Whole-Foods, Plant-Based Diet Alleviates the Symptoms of Osteoarthritis. Chelsea M. Clinton, Shanley O’Brien, Junwen Law, Colleen M. Renier, and Mary R. Wendt. [↩]
- Healthy Joints: Dr Greger [↩]
- Preventing Arthritis. Michael Greger M.D. FACLM September 16th, 2008 Volume 2. [↩]
- A. Hailu, S.F. Knutsen, & G.E. Fraser. Associations between meat consumption and the prevalence of degenerative arthritis and soft tissue disorders in the Adventist health study, California U.S.A. J Nutr Health Aging, 10(1):7-14, 2006. [↩]
- Diet & Rheumatoid Arthritis. Michael Greger M.D. FACLM September 20th, 2010 Volume 4 [↩]
- PCRM: Focus on plant-based foods to ease arthritis pain. [↩]
- Which Athlete Ate the Most Nitrates… [↩]
- Nutritionfacts.org: Nitrates [↩]
- CNS: Nitric Oxide & Dietary Nitrate: Another Reason to Eat Your Vegetables [↩]
- Front Pharmacol. 2013; 4: 71. The effects of cocoa on the immune system. Francisco J. Pérez-Cano, Malen Massot-Cladera, Àngels Franch, Cristina Castellote, and Margarida Castell. [↩]
- Nutrients. 2016 Jun; 8(6): 321. Impact of Cocoa Consumption on Inflammation Processes—A Critical Review of Randomized Controlled Trials. Sabine Ellinger, Peter Stehle. [↩]
- Clin Rheumatol. 2016; 35(12): 2901–2908. Dietary intake and risk of rheumatoid arthritis—a cross section multicenter study. Jing He, et al. [↩]
- Front Nutr. 2017; 4: 52. Managing Rheumatoid Arthritis with Dietary Interventions. Shweta Khanna, Kumar Sagar Jaiswal, Bhawna Gupta. [↩]
- What is the evidence for a role for diet and nutrition in osteoarthritis?Sally Thomas Heather Browne Ali Mobasheri Margaret P Rayman. Rheumatology, Volume 57, Issue suppl_4, 1 May 2018, Pages iv61–iv74. [↩]
- Arthritis Research UK: Are there any links between tomatoes and worsening arthritis? [↩]
- ScienceDaily: Garlic could protect against hip osteoarthritis. December 16, 2010. King’s College London. [↩]
- Friday, January 29. Arthritis Today Magazine. Research Shows Apples Can Cut Cholesterol and Inflammation [↩]
- Vitamin C Supplements vs An Apple [↩]
- Arthritis Research UK: Has eating bananas helped with my arthritis pain? [↩]
- Athletic Performance & Physical Damage on Plant-Based Diets [↩]
- WFPB Eating to Prevent Sports Injuries [↩]
- Exercise vs Whole Food Plant-Based Diet [↩]
- Good Bacteria Produce Butyrate [↩]
- Gout, Uric Acid, Urea, Purines & Plant-Based Diets [↩]
- Wholism vs Reductionism – Not Just a War of Words [↩] [↩]
- Campbell, T. Colin. Whole: Rethinking the Science of Nutrition (p. 97). BenBella Books, Inc.. Kindle Edition. [↩]