One of my clients emailed me to say that he was concerned about his blood pressure. On the WFPB programme for nearly four weeks, his blood pressure has been dropping consistently from around 160/100 when he started, to 113/78 two days ago. Then it looked like it was starting to rise again. I sensed some panic in his tone…
When I looked at his nutritional/lifestyle diary for the past days I could see the problem – sleep or rather the lack of it.
A recent study of US citizens found that 1 in 3 were chronically sleep deprived. It is likely figures for other Western countries are similar. Sleep – or, rather, the lack of it – is a BIG problem for many people.
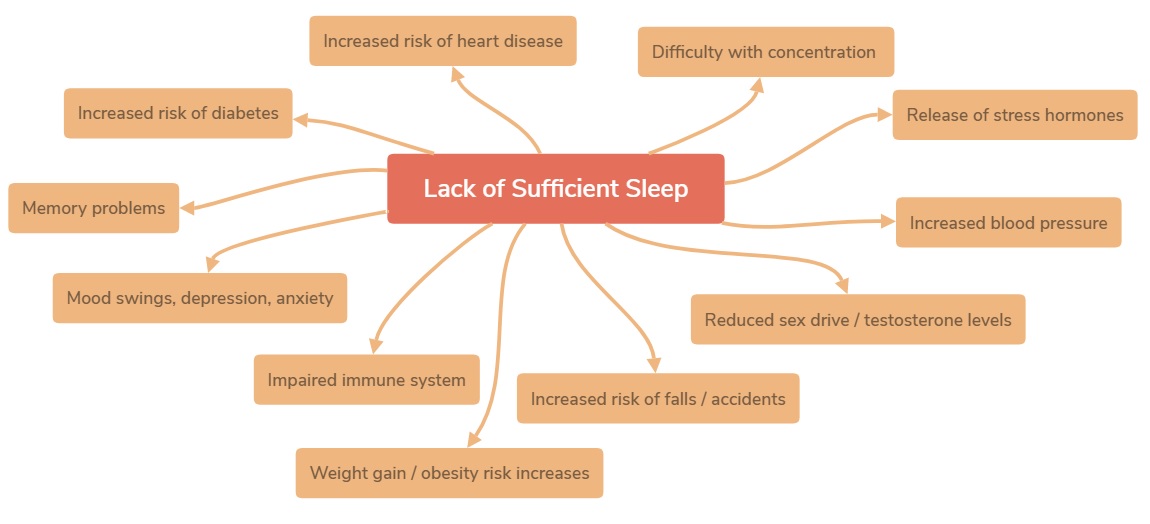
Health conditions associated with lack of sleep
And what few fully appreciate is that blood pressure (BP) rises if you have insufficient sleep. And raised BP is not all. The following are also associated with sleep deficiency:
- Raised blood pressure / heart rate (hypertension)
- Cancer
- Alzheimer ‘s disease (AD)
- General neurodegenerative disorders
- Dementia
- Coronary heart disease (CHD)
- Stroke
- Childhood obesity
- Adult obesity
- Diabetes
- Metabolic syndrome
- Immunological changes
- Depression
- Increased pain sensitivity (hyperalgesia)
- Chronic skin ageing
- Sexual dysfunction
- Increased susceptibility to the common cold
- All-cause mortality
- Impaired school readiness
- Increased aggression/violent tendencies
- Increased accident risk
- Increased sick leave from work
- Impaired memory & Reasoning
- Release of stress hormones
Blog Contents
Suggestions for improving quality of sleep
So, how do we ensure that we stand the best chance of getting enough good quality sleep? The following are associated with improved sleep patterns according to both third-party studies and my own professional/personal experience:
- Improve your diet, high fibre/low saturated fat
- Eat more cherries and kiwi fruit
- Increase daily physical exercise
- Reduce alcohol consumption
- Reduce light in bedroom (eye masks)
- Reduce noise (earplugs)
- Use mindfulness techniques to get back to sleep (more about mindfulness in future posts)
A little more detail…
More on the benefits of plant-based diets
More advice on optimal amounts of sleep.
More on sleep and the immune system.
More on the relationship between cherries, kiwifruit and sleep.
A note about melatonin
Melatonin is a hormone secreted at night by the pineal gland in the center of our brain to help regulate our circadian rhythm. Supplements are used to prevent and reduce jet lag. MIT got the patent to use melatonin to help people sleep. But melatonin “is not only produced in the pineal gland—it is also naturally present in edible plants.
For more information on melatonin.
The above is by no means meant to be a comprehensive list of the chronic health conditions associated with sleep deficiency; nor have I provided a definitive list of suggestions for improving sleep quality. If it forms a basis for discussion or for you to undertake your own research (and send me the findings, please!) then that is a sufficient achievement.
What I will add is that the four cornerstones of health that I continue to mention (diet, sleep, exercise and stress-avoidance) are all a part of the wholistic approach that I consider optimal for human health and well-being.
Diet is perhaps the most important element in all of this, since it forms the basis for being able to sleep well, recover from and endure exercise, and enjoy a positive, stress-reduced mental attitude. Part of the reason why it is able to do this is because it is fundamental to maintaining the body in a state of homeostasis (balance), rather than having to constantly detoxify, protect and repair itself from the inferior “foods” we have so often forced our poor bodies to eat.
Wholistic = Diet+Exercise+Sleep+Stress Reduction…They work together. They compliment one another.
A few final words from Dr Neal Barnard about high-protein foods and sleep
“While many people believe that high-protein meals are key to getting a good night’s rest, the opposite is true. High-protein foods block the brain’s ability to produce serotonin. Because high-protein foods contain more amino acids, tryptophan—the amino acid that eventually turns into serotonin—is crowded out of the brain. As a result, high-protein foods will leave you feeling alert.
High-protein plant-based foods, like tofu, beans, and lentils, are very nutritious. But if you’re having trouble sleeping, try eating these foods earlier in the day. You’ll feel more alert during the day, while favoring carbohydrates later on can help you rest at night.”
Dr Neal Barnard in his own words:
References
Health conditions associated with lack of sleep (in addition to the above links)
Osamu Tochikubo, Akihiko Ikeda, Eiji Miyajima, Masao Ishii. https://doi.org/10.1161/01.HYP.27.6.1318. Hypertension. 1996;27:1318-1324.
Originally published June 1, 1996. Effects of Insufficient Sleep on Blood Pressure Monitored by a New Multibiomedical Recorder.
Noguti J, Andersen ML, Cirelli C, Ribeiro DA. Sleep Breath. 2013 Sep;17(3):905-10. doi: 10.1007/s11325-012-0797-9. Epub 2013 Feb 1. Oxidative stress, cancer, and sleep deprivation: is there a logical link in this association?
Redeker NS, Pigeon WR, Boudreau EA. Support Care Cancer. 2015 Apr;23(4):1145-55. doi: 10.1007/s00520-014-2537-0. Epub 2014 Dec 16.
Incorporating measures of sleep quality into cancer studies.
Wang P, Ren FM, Lin Y, Su FX, Jia WH, Su XF, Tang LY, Ren ZF. Sleep Med. 2015 Apr;16(4):462-8. doi: 10.1016/j.sleep.2014.11.017. Epub 2015 Feb 3. Night-shift work, sleep duration, daytime napping, and breast cancer risk.
Olsson M, Ärlig J, Hedner J, Blennow K1, Zetterberg H. Sleep. 2018 Feb 7. doi: 10.1093/sleep/zsy025. Sleep Deprivation and CSF Biomarkers for Alzheimer Disease.
Ju YE, McLeland JS, Toedebusch CD, Xiong C, Fagan AM, Duntley SP, Morris JC, Holtzman DM. AMA Neurol. 2013 May;70(5):587-93. doi: 10.1001/jamaneurol.2013.2334. Sleep quality and preclinical Alzheimer disease.
Malhotra RK. Sleep Med Clin. 2018 Mar;13(1):63-70. doi: 10.1016/j.jsmc.2017.09.006. Epub 2017 Nov 10. Neurodegenerative Disorders and Sleep.
Holingue C, Wennberg A, Berger S, Polotsky VY, Spira AP. Metabolism. 2018 Jan 31. pii: S0026-0495(18)30029-5. doi: 10.1016/j.metabol.2018.01.021. Disturbed Sleep and Diabetes: A Potential Nexus of Dementia Risk.
Lao XQ, Liu X, Deng HB, Chan TC, Ho KF, Wang F, Vermeulen R, Tam T, Wong MCS, Tse LA, Chang LY, Yeoh EK. J Clin Sleep Med. 2018 Jan 15;14(1):109-117. doi: 10.5664/jcsm.6894. Sleep Quality, Sleep Duration, and the Risk of Coronary Heart Disease: A Prospective Cohort Study With 60,586 Adults.
Solarz DE, Mullington JM, Meier-Ewert HK. Front Biosci (Elite Ed). 2012 Jun 1;4:2490-501. Sleep, inflammation and cardiovascular disease.
Ancoli-Israel S, DuHamel ER, Stepnowsky C, Engler R, Cohen-Zion M, Marler M. Chest. 2003 Oct;124(4):1400-5. The relationship between congestive heart failure, sleep apnea, and mortality in older men.
Fletcher EC. Monaldi Arch Chest Dis. 1996 Feb;51(1):77-80. Obstructive sleep apnoea and cardiovascular morbidity.
Patyar S, Patyar RR.. J Stroke Cerebrovasc Dis. 2015 May;24(5):905-11. doi: 10.1016/j.jstrokecerebrovasdis.2014.12.038. Epub 2015 Mar 25. Correlation between Sleep Duration and Risk of Stroke.
Miller MA, Kruisbrink M, Wallace J, Ji C, Cappuccio FP. Sleep. 2018 Feb 1. doi: 10.1093/sleep/zsy018. Sleep Duration and Incidence of Obesity in Infants, Children and Adolescents: A Systematic Review and Meta-Analysis of Prospective Studies.
Bell JF, Zimmerman FJ. Arch Pediatr Adolesc Med. 2010 Sep;164(9):840-5. doi: 10.1001/archpediatrics.2010.143. Shortened nighttime sleep duration in early life and subsequent childhood obesity.
Hart CN, Jelalian E. Behav Sleep Med. 2008;6(4):251-67. doi: 10.1080/15402000802371379. Shortened sleep duration is associated with pediatric overweight.
Taveras EM, Gilliman MW, Pena MM, Redline S, Rifas Shiman SL. Jun;133(6):1013-22. Pediatrics. 2014. Chronic Sleep Curtailment and Adiposity.
Patel SR, Hu FB. Obesity (Silver Spring). 2008; 16:643-53. Short sleep duration and weight gain: a systematic review.
PatelSR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Am J Epidemiol.2006; 164:947-54. Association between reduced sleep and weight gain in women.
Kim CW, Chang Y, Sung E, Ryu S.. Diabet Med. 2017 Nov;34(11):1591-1598. doi: 10.1111/dme.13432. Epub 2017 Aug 14. Sleep duration and progression to diabetes in people with prediabetes defined by HbA1c concentration.
Briançon-Marjollet A, Weiszenstein M, Henri M, Thomas A, Godin-Ribuot D, Polak J. Diabetol Metab Syndr. 2015 Mar 24;7:25. doi: 10.1186/s13098-015-0018-3. eCollection 2015. The impact of sleep disorders on glucose metabolism: endocrine and molecular mechanisms.
Orzeł-Gryglewska J. Int J Occup Med Environ Health. 2010;23(1):95-114. doi: 10.2478/v10001-010-0004-9. Consequences of sleep deprivation. [Immunological changes]
Riemann D, Baglioni C, Spiegelhalder K. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2011 Dec;54(12):1296-302. doi: 10.1007/s00103-011-1378-y. [Lack of sleep and insomnia. Impact on somatic and mental health]. [Article in German]
Riemann D. Sleep Med. 2007 Dec;8 Suppl 4:S15-20. doi: 10.1016/S1389-9457(08)70004-2. Insomnia and comorbid psychiatric disorders.
Papadimitriou GN, Linkowski P. Int Rev Psychiatry. 2005 Aug;17(4):229-36. Sleep disturbance in anxiety disorders.
Roehrs T, Hyde M, Blaisdell B, Greenwald M, Roth T. Sleep. 2006 Feb;29(2):145-51. Sleep loss and REM sleep loss are hyperalgesic. [Increased cute/chronic pain sensitivity]
Alexandre C, Latremoliere A, Ferreira A, Miracca G, Yamamoto M, Scammell TE, Woolf CJ. Nat Med. 2017 Jun;23(6):768-774. doi: 10.1038/nm.4329. Epub 2017 May 8. Decreased alertness due to sleep loss increases pain sensitivity in mice.
Oyetakin-White P, Suggs A, Koo B, Matsui MS, Yarosh D, Cooper KD, Baron ED. Clin Exp Dermatol. 2015 Jan;40(1):17-22. doi: 10.1111/ced.12455. Epub 2014 Sep 30. Does poor sleep quality affect skin ageing?
Pastuszak AW, Moon YM, Scovell J, Badal J, Lamb DJ, Link RE, Lipshultz LI. Urology. 2017 Apr;102:121-125. doi: 10.1016/j.urology.2016.11.033. Epub 2016 Dec 14. Poor Sleep Quality Predicts Hypogonadal Symptoms and Sexual Dysfunction in Male Nonstandard Shift Workers.
Hirotsu C, Soterio-Pires JH, Tufik S, Andersen ML. Int J Impot Res. 2017 May;29(3):126. doi: 10.1038/ijir.2017.1. Epub 2017 Feb 16. Sleep disturbance and sexual dysfunction in postmenopausal women.
Opstad PK.. J Clin Endocrinol Metab. 1992 May;74(5):1176-83. Androgenic hormones during prolonged physical stress, sleep, and energy deficiency. 9 [Adrenal & Testicular Androgens]
Sheldon Cohen, PhD, William J. Doyle, PhD, Cuneyt M. Alper, MD, Denise Janicki-Deverts, PhD, and Ronald B. Turner, MD. Arch Intern Med. Author manuscript; available in PMC 2010 Jan 12. Published in final edited form as:Arch Intern Med. 2009 Jan 12; 169(1): 62–67.
doi: 10.1001/archinternmed.2008.505. Sleep Habits and Susceptibility to the Common Cold.
Liu TZ, Xu C, Rota M, Cai H, Zhang C, Shi MJ, Yuan RX, Weng H, Meng XY, Kwong JS, Sun X. Sleep Med Rev. 2017 Apr;32:28-36. doi: 10.1016/j.smrv.2016.02.005. Epub 2016 Mar 3. Sleep duration and risk of all-cause mortality: A flexible, non-linear, meta-regression of 40 prospective cohort studies.
Tso W, Rao N, Jiang F, Li AM, Lee SL, Ho FK, Li SL, Ip P. J Pediatr. 2016 Feb;169:266-71. doi: 10.1016/j.jpeds.2015.10.064. Epub 2015 Nov 19. Sleep Duration and School Readiness of Chinese Preschool Children.
Street NW, McCormick MC, Austin SB, Slopen N4 Habre R, Molnar BE. Sleep Health. 2016 Jun;2(2):129-135. doi: 10.1016/j.sleh.2016.03.002. Epub 2016 Apr 18. Sleep duration and risk of physical aggression against peers in urban youth.
Luyster FS, Strollo PJ Jr, Zee PC, Walsh JK; Boards of Directors of the American Academy of Sleep Medicine and the Sleep Research Society. Sleep. 2012 Jun 1;35(6):727-34. doi: 10.5665/sleep.1846. Sleep: a health imperative. [Increased risk of fatal accidents]
Philip P, Akerstedt T. Sleep Med Rev. 2006 Oct;10(5):347-56. Epub 2006 Aug 22. Transport and industrial safety, how are they affected by sleepiness and sleep restriction?
Akerstedt T, Kecklund G, Alfredsson L, Selen J. J Sleep Res. 2007 Dec;16(4):341-5. Predicting long-term sickness absence from sleep and fatigue.
Lim J, Dinges DF. Psychol Bull. 2010 May;136(3):375-89. doi: 10.1037/a0018883. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables.
Esposito MJ, Occhionero M1, Cicogna P. Sleep. 2015 Nov 1;38(11):1823-6. doi: 10.5665/sleep.5172. Sleep Deprivation and Time-Based Prospective Memory.
Lima AM, de Bruin VM, Rios ER, de Bruin PF. Naunyn Schmiedebergs Arch Pharmacol. 2014 May;387(5):399-406. doi: 10.1007/s00210-013-0955-z. Epub 2014 Jan 15. Differential effects of paradoxical sleep deprivation on memory and oxidative stress.
Eun Yeon Joo, Cindy W Yoon, Dae Lim Koo, Daeyoung Kim and Seung Bong Hong/ J Clin Neurol. 2012 Jun;8(2):146-150. English.
Published online June 29, 2012. https://doi.org/10.3988/jcn.2012.8.2.146. Adverse Effects of 24 Hours of Sleep Deprivation on Cognition and Stress Hormones.
Suggestions for improving quality of sleep (in addition to the above links)
Nutr Res. 2012 May;32(5):309-19. doi: 10.1016/j.nutres.2012.03.009. Epub 2012 Apr 25. Peuhkuri K, Sihvola N, Korpela R. Diet promotes sleep duration and quality.
St-Onge MP, Roberts A, Shechter A, Choudhury AR. J Clin Sleep Med. 2016 Jan;12(1):19-24. doi: 10.5664/jcsm.5384. Fiber and Saturated Fat Are Associated with Sleep Arousals and Slow Wave Sleep.
G. Howatson, P. G. Bell, J. Tallent, B. Middleton, M. P. McHugh, J. Ellis. Eur J Nutr 2012 51(8):909 – 916. Effect of tart cherry juice (Prunus cerasus) on melatonin levels and enhanced sleep quality.
H.-H. Lin, P.-S. Tsai, S.-C. Fang, J.-F. Liu. Asia Pac J Clin Nutr 2011 20(2):169 – 174. Effect of kiwifruit consumption on sleep quality in adults with sleep problems.
Brand S, Gerber M, Beck J, Hatzinger M, Pühse U, Holsboer-Trachsler E. J Adolesc Health. 2010 Feb;46(2):133-41. doi: 10.1016/j.jadohealth.2009.06.018. Epub 2009 Aug 18. High exercise levels are related to favorable sleep patterns and psychological functioning in adolescents: a comparison of athletes and controls.
Thakkar MM, Sharma R, Sahota P. Alcohol. 2015 Jun;49(4):299-310. doi: 10.1016/j.alcohol.2014.07.019. Epub 2014 Nov 11. Alcohol disrupts sleep homeostasis.
Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol Clin Exp Res. 2013 Apr;37(4):539-49. doi: 10.1111/acer.12006. Epub 2013 Jan 24. Review. Alcohol and sleep I: effects on normal sleep.
Jeanne F. Duffy, M.B.A., Ph.D.a, and Charles A. Czeisler, Ph.D., M.D. Sleep Med Clin. Author manuscript; available in PMC 2010 Jun 1.
Published in final edited form as: Sleep Med Clin. 2009 Jun; 4(2): 165–177. doi: 10.1016/j.jsmc.2009.01.004. Effect of Light on Human Circadian Physiology
Giménez MC, Geerdinck LM, Versteylen M, Leffers P, Meekes GJ, Herremans H, de Ruyter B, Bikker JW, Kuijpers PM, Schlangen LJ. J Sleep Res. 2017 Apr;26(2):236-246. doi: 10.1111/jsr.12470. Epub 2016 Nov 10. Patient room lighting influences on sleep, appraisal and mood in hospitalized people.
Yamauchi M, Jacono FJ, Fujita Y, Kumamoto M, Yoshikawa M, Campanaro CK, Loparo KA, Strohl KP, Kimura H. Sleep Breath. 2014 Dec;18(4):829-35. doi: 10.1007/s11325-014-0951-7. Epub 2014 Feb 13. Effects of environment light during sleep on autonomic functions of heart rate and breathing.
Jones C, Dawson D. Nurs Crit Care. 2012 Sep-Oct;17(5):247-54. doi: 10.1111/j.1478-5153.2012.00501.x. Epub 2012 May 15. Eye masks and earplugs improve patient’s perception of sleep.
Hu RF, Jiang XY, Hegadoren KM, Zhang YH. Crit Care. 2015 Mar 27;19:115. doi: 10.1186/s13054-015-0855-3. Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial.
Zaharna M, Guilleminault C. Noise Health. 2010 Apr-Jun;12(47):64-9. doi: 10.4103/1463-1741.63205. Sleep, noise and health: review.
Andrew J.HowellNancy L.DigdonKarenBuro. Personality and Individual Differences (ISSID). Volume 48, Issue 4, March 2010, Pages 419-424. Mindfulness predicts sleep-related self-regulation and well-being.
Huang X, Mazza G. Crit Rev Food Sci Nutr. 2011 Apr;51(4):269-84. doi: 10.1080/10408398.2010.529193. Application of LC and LC-MS to the analysis of melatonin and serotonin in edible plants.
Kehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, Inaba Y, Tamakoshi A; JACC Study Group. Association of Sleep Duration with Mortality from Cardiovascular Disease and Other Causes for Japanese Men and Women: the JACC Study. Sleep. 2009 Mar;32(3):295-301.