You hear a lot about diabetes, but you possibly do not get detailed information about the actual processes involved in its development, nor about the specific and, frankly, disturbing consequences of living with this debilitating disease.
This blog goes into some detail and shows some disturbing photos of the results of diabetes. If you do not wish to see these images, you can contact me for a copy of this blog without any images.
I have a very specific reason for covering this issue in such vivid detail: It is no exaggeration to claim that diabetes, particularly but not exclusively type 2 diabetes, is becoming an epidemic in the western world, and not just starting in middle age, but appearing in younger generations. There is solid and reliable evidence that this is due to the western diet – dependent on animal products, low-fibre, high-sugar and fat processed foods, and deficient in whole plant foods.
I will present other articles in defence of this assertion but, for the time being, I want to focus on the disturbing reality of those people who live with diabetes – a largely avoidable chronic disease which has been shown to be both avoidable and reversible by eating a whole food plant-based diet.
Diabetes mellitus (1.) (DM) is caused by complete absence, relative deficiency of, or resistance to the hormone insulin.
The most common forms of DM are categorised as type 1 diabetes mellitus or type 2 diabetes mellitus.
Blog Contents
Definitions
Type 1 diabetes mellitus
- previously known as insulin-dependent diabetes mellitus (IDDM)
- mainly occurring in children and young adults
- onset is usually sudden and can be life threatening
- severe deficiency or absence of insulin secretion due to destruction of β-islet cells of the pancreas
- treatment with injections of insulin is required
- usually evidence of an autoimmune mechanism that destroys the β-islet cells
- genetic predisposition and environmental factors, including viral infections. Diet/lifestyle are also implicated
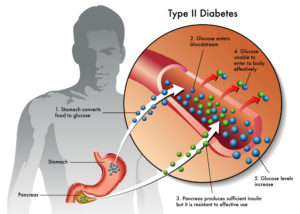
Type 2 diabetes mellitus
- previously known as non-insulin-dependent diabetes mellitus (NIDDM)
- most common form of diabetes, accounting for about 90% of cases
- causes are multifactorial and predisposing factors include:
- obesity
- sedentary lifestyle
- increasing age: predominantly affecting middle-aged and older adults but increasingly affecting younger groups
- genetic factors
- onset is gradual, often over many years
- frequently undetected until signs are found on routine investigation or a complication occurs
- insulin secretion may be below or above normal
- deficiency of glucose inside body cells occurs despite hyperglycaemia (high blood sugar) and high insulin level, possibly because of:
- insulin resistance, i.e. changes in cell membranes that block insulin-assisted movement of glucose into cells.
- treatment involves diet and/ or drugs, although sometimes insulin injections are required
Pathophysiology (disease processes) (2.) of DM
1. Raised plasma glucose level
After eating a carbohydrate-rich meal the plasma glucose level remains high because:
- cells are unable to take up and use glucose from the bloodstream, despite high plasma levels
- conversion of glucose to glycogen in the liver and muscles is diminished
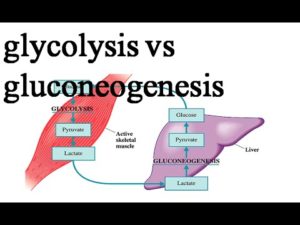
- gluconeogenesis (non-carbohydrate glucose production) (3.) from protein, in response to deficiency of intracellular glucose.
2a. Glycosuria (sugar in urine) (4.) and 2b. Polyuria (excessive urination) (5.)
a. Glycosuria results in electrolyte imbalance and excretion of urine with a high specific gravity.
b. Polyuria leads to dehydration, extreme thirst (polydipsia) and increased fluid intake.
3. Weight loss
Cells “starved” of glucose – leading to:
- gluconeogenesis from amino acids/body protein, causing muscle wasting/tissue breakdown/further increases in blood glucose
- catabolism of body fat, releasing some of its energy and excess production of ketone bodies (6.)
- very common in type 1 DM
- sometimes occurs in type 2 DM
4. Ketosis (7.)and ketoacidosis (8.)
- generally affects people with type 1 DM – in absence of insulin to promote normal intracellular glucose metabolism, alternative energy sources must be used instead and increased breakdown of fat occurs. Results in:
- excessive production of weakly acidic ketone bodies, which can be used for metabolism by the liver
- ketosis develops as ketone bodies accumulate.
- excretion of ketones is via the urine (ketonuria) and/ or the lungs giving the breath a characteristic smell of acetone or ‘pear drops’.
- ketoacidosis develops owing to increased insulin requirement or increased resistance to insulin.
- if untreated it can lead to:
- increasing acidosis (↓ blood pH) due to accumulation of ketoacids
- increasing hyperglycaemia
- hyperventilation as the lungs excrete excess hydrogen ions as CO2
- acidification of urine – the result of kidney buffering
- polyuria as the renal threshold for glucose is exceeded
- dehydration and hypovolaemia (9.) (↓ BP and ↑ pulse) – caused by polyuria
- disturbances of electrolyte balance accompanying fluid loss:
- hyponatraemia (10.) (↓ plasma sodium) and hypokalaemia (11.) (↓ plasma potassium)
- confusion, coma and death
5, Acute complications of DM
- Effects and consequences of diabetic ketoacidosis are outlined above
- Hypoglycaemic coma:
- occurs when insulin administered is in excess of that needed to balance the food intake and expenditure of energy
- sudden onset and may be the result of:
- accidental overdose of insulin
- delay in eating after insulin administration
- drinking alcohol on an empty stomach
- strenuous exercise
- insulin-secreting tumour
- Common signs and symptoms of hypoglycaemia include:
- drowsiness
- confusion
- speech difficulty
- sweating
- trembling
- anxiety
- rapid pulse.
- May progress rapidly to coma without treatment
- Rapid recovery with treatment M
6. Long-term complications of DM (Type 1 and type 2)
- Cardiovascular disturbances
- DM is a significant risk factor for cardiovascular disorders
- Blood vessel abnormalities (angiopathies) may still occur even when the disease is well controlled by medication
- Diabetic macroangiopathy (12.). Most common lesions are:
- atheroma
- calcification of the tunica media of the large arteries. Resulting in:
- Often serious and fatal consequences for Type 1 diabetes at a relatively early age.
- For both Type 1 and Type 2, the most common consequences are serious and often fatal:
- ischaemic heart disease (angina and myocardial infarction)
- stroke
- peripheral vascular disease.

- Diabetic microangiopathy (13.). This affects small blood vessels and can result in:
- thickening of the epithelial basement membrane of arterioles, capillaries and, sometimes, venules. Leading to:
- Peripheral vascular disease, progressing to gangrene and ‘diabetic foot’
- Diabetic retinopathy (14.)
- Visual impairment
- Diabetic nephropathy (15.) and chronic renal failure
- Peripheral neuropathy (16.) causing sensory deficits and motor weakness
- Infection
- DM predisposes to infection, especially by bacteria and fungi, possibly because phagocyte activity is depressed by insufficient intracellular glucose. Infection may cause:
- boils and carbuncles
- vaginal candidiasis (17.)
- pyelonephritis (18.)
- diabetic foot
- DM predisposes to infection, especially by bacteria and fungi, possibly because phagocyte activity is depressed by insufficient intracellular glucose. Infection may cause:
- Renal failure
- This is due to diabetic nephropathy (15.) and is a common cause of death.
- thickening of the epithelial basement membrane of arterioles, capillaries and, sometimes, venules. Leading to:

- Visual impairment and blindness
- Diabetic retinopathy (14.)
- commonest cause of blindness in adults between 30 and 65 years in developed countries
- increases the risk of early development of cataracts
- increase the risk of early development of other visual disorders
- Diabetic retinopathy (14.)
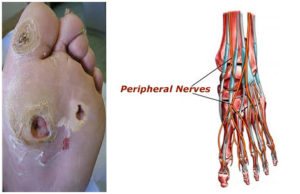
- Diabetic foot
- Many factors commonly present in DM contribute to the development of this serious situation:
- disease of large and small blood vessels impairs blood supply to and around the extremities
- if peripheral neuropathy (16.) is present:
- sensation is reduced
- a small injury to the foot may go unnoticed, especially when there is visual impairment
- in DM healing is slower and injuries easily worsen if aggravated, e.g. by chafing shoes
- often become infected
- an ulcer may form
- healing process is lengthy, if at all
- in severe cases the injured area ulcerates and enlarges
- may become gangrenous
- sometimes to the extent that amputation is required.
- Many factors commonly present in DM contribute to the development of this serious situation:
Why risk or suffer from this truly dreadful disease if the most effective prevention and cure (a WFPB diet) has no side-effects other than improved overall health?
What an unfathomable species we are…

Glossary
- ” Of or pertaining to honey” – https://en.wiktionary.org/wiki/mellitus.
- “The physiological processes associated with disease or injury” – https://en.wiktionary.org/wiki/pathophysiology
- “The metabolic process in which glucose is formed, mostly in the liver, from non-carbohydrate precursors” – https://en.wiktionary.org/wiki/gluconeogenesis
- “The presence of sugars (especially glucose) in the urine, often as a result of diabetes mellitus” – https://en.wiktionary.org/wiki/glycosuria
- “The production of an abnormally large amount of urine; one symptom of diabetes” – https://en.wiktionary.org/wiki/polyuria
- “Any of several compounds that are intermediates in the metabolism of fatty acids” – https://en.wiktionary.org/wiki/ketone_body#English.
- “A metabolic state in which the body produces ketones to be used as fuel by some organs so that glycogen can be reserved for organs that depend on it. This condition occurs during times of fasting, starvation, or while on a ketogenic weight-loss diet” – https://en.wiktionary.org/wiki/ketosis.
- “A severe form of ketosis, most commonly seen in diabetics, in which so much ketone is produced that acidosis occurs” – https://en.wiktionary.org/wiki/ketoacidosis.
- “A state of decreased blood volume” – https://en.wiktionary.org/wiki/hypovolemia#English.
- “An abnormally low concentration of sodium (or salt) in blood plasma” – https://en.wiktionary.org/wiki/hyponatremia#English.
- “The condition of having an abnormally low concentration of potassium ions in the blood” – https://en.wiktionary.org/wiki/hypokalemia#English.
- “Angiopathy of the larger blood vessels” – https://en.wiktionary.org/wiki/macroangiopathy.
- “Angiopathy of the small blood vessels” – https://en.wiktionary.org/wiki/microangiopathy.
- “Non-inflammatory disease of the retina” – https://en.wiktionary.org/wiki/retinopathy.
- “Damage to, disease of, or abnormality of the kidneys” – https://en.wiktionary.org/wiki/nephropathy.
- “Any disease of the peripheral nervous system” – https://en.wiktionary.org/wiki/neuropathy.
- “A fungal infection of any of the Candida (yeast) species” – https://en.wiktionary.org/wiki/candidiasis. Also called “thrush”.
- “An ascending urinary tract infection that has reached the pelvis of the kidney” – https://en.wiktionary.org/wiki/pyelonephritis.
Main source of material: Waugh, Anne; Grant, Allison. Ross & Wilson Anatomy and Physiology in Health and Illness E-Book (p. 236-8). Elsevier Health Sciences. Kindle Edition.
