
An October 2017 double-blind, placebo-controlled and randomised pilot study1 at the University of Almería, Spain appears to have been the first to evaluate the effects of probiotics in fibromyalgia syndrome (often abbreviated to FMS). They looked at whether interventions with probiotics, in order to change the gut microbiota, could improve the symptoms of this debilitating disease. Their results may be very encouraging for those who believe that “you are what you eat” and would agree with that ancient sage Hippocrates when he said “Let food be thy medicine, and medicine thy food“.
The studies covered in this blog are covered in an effort to provide a wide-range of research material and, hence, a range of viewpoints on the subject matter. My own personal opinions are expressed in [square brackets] throughout.
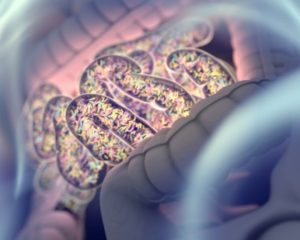
FMS is a chronic, generalised and diffuse pain disorder accompanied by other symptoms such as emotional and cognitive deficits. There would be little surprise if gut microbiota were intrinsically linked to this condition when you consider that FMS patients show a high prevalence of gastrointestinal symptoms.
As pointed out in other blogs2 , gut microbiota are increasingly considered to be involved in the regulation of brain processes through the gut-microbiota-brain axis, thereby modulating mood, motivation, cognitive functions, and so on. This study used probiotics as a new treatment that could improve the physical, psychological and cognitive state in FMS; being that they found no other experimental evidence to substantiate or refute this possible therapeutic approach being used with FMS to date.
Blog Contents
Method
The intervention consisted of the administration of two different combinations of multispecies probiotics (provided by commercial pharmaceutical companies), or a placebo taken every day for eight weeks. The probiotics used were:
- Probiotic 1
- S. thermophiles
- S. faecium
- L. acidophilus
- L. rhamnosus
- L. casei
- L. bulgaricus
- B. bifidum
- B. infantis
- Probiotic 2
- L. rhamnosus GG® [A trademarked bacterium is perhaps a worrying sign of things to come…]
- Casei
- Acidophilus
- B. bifidus
Expected Results
Primary expected outcome: MS patients’ cognition will, after eight weeks of probiotic treatment, show a better performance on impulsive choice and decision-making, as well as on working memory and attentional control.
Secondary expected outcomes: mean changes between baseline/post=intervention in body composition, pain level, and emotional state.
Additional expected outcomes: changes in physiological measures – specifically, free cortisol concentration in urine and stool faecal samples.
Whilst the results of this trial are still awaited, the researchers list the following experimental findings which may suggest that their anticipated results will not be too far away from their stated expectations:
- Ingestion of probiotics positively affects the host’s health by improving the microbial balance3 and may positively affect cognitive and psychological processes via the gut-brain axis4
- Possible mechanisms of action of probiotics include:
- competition against the pathogenic bacteria to bind to the intestinal epithelial cells
- enhancement of the intestinal epithelial barrier function
- inhibition of pathogens’ growth by secretion of antimicrobial peptides
- augmentation of the production of serum IgA 5 6
- Probiotics may also affect the central nervous system through the gut-brain axis via:
- For instance, some probiotics have been shown to induce an elevation of tryptophan levels in plasma9 , which is a precursor of serotonin
- Serotonin has been implicated in emotional processes, cognition, motor function and pain, as well as in neuroendocrine functions, such as food intake, circadian rhythms and reproductive activity10
- A very important practical implication of this is that probiotics may then produce health benefits in patients suffering from neuropsychiatric disorders7
- Therefore, FMS is one of the target populations. FMS patients show a seemingly altered microbiome11 12 . Their symptoms include chronic, generalised and diffuse pain disorders, as well as fatigue, depression, sleeping disorders13 , self-reported reduced mental performance14 15 16 17 and cognitive deficits in inhibition and decision-making processes18
- Previous studies with probiotics in populations with a great comorbidity with FMS, like CFS (chronic fatigue syndrome) and IBS (irritable bowel syndrome)19 20 21 , have reported beneficial effects after treatment in quality of life7 , pain severity22 , reduced inflammation23 , and emotional symptoms like anxiety24 .
 Fibromyalgia, IBS & SIBO
Fibromyalgia, IBS & SIBO
An October 2017 updated article in News: Medical Life Sciences25 makes some interesting observations about fibromyalgia and the small intestine.
It points out that IBS has been linked to the occurrence of small intestine bacterial overgrowth (SIBO), a condition where normal colonic flora overgrow into the small intestine and cause disruption of normal intestinal bacterial patterns.
The author considers that connection suggests that fibromyalgia is also associated with SIBO. The evidence for this is based on the finding that correcting the latter with antibiotic therapy also lead to clinical improvements in bowel symptoms in these patients.
Mechanisms involved in the fibromyalgia-SIBO link
Mechanism 1 – Several studies are mentioned (without links) which claim that both fibromyalgia and IBS yield abnormal lactulose breath tests (LBT) – tests for bacterial overgrowth which is almost always positive in fibromyalgia patients. The idea is that endotoxins produced by overgrown bacteria are responsible for the hyperalgesia26) is an increased sensitivity to pain, which may be caused by damage to nociceptors or peripheral nerves.)) by increasing pain perception in the body.
Mechanism 2 – Another mechanism of pain production is bacterial translocation, common in SIBO and results in production of endotoxins which provoke the production of the tumour necrosis factor, leading to systemic effects.
Fibromyalgia and IBS have many common features as regards the bowel disturbances, but it’s also the case that there can be significant some variations in clinical features. What accounts for this variation? It could be due to differences in the host, or that different patterns of bacterial overgrowth may occur in different conditions. For instance, hydrogen breath testing in individuals with fibromyalgia shows a far higher level of hydrogen production when compared with IBS patients even when both are LBT positive27 , and this may reflect a larger number of small intestinal bacteria.
Treatment of Gut-Related Fibromyalgia
Recent research has shown significant correlations between the fibromyalgia and increased intestinal permeability. The latter permeability is related to SIBO, and so doctors are increasingly considering that the following measures may be helpful:
Including the following foods in the diet:
- Fermentable fibre28 (e.g. sweet potato, oats, barley, fruit & vegetables)
- Fermented foods such as sauerkraut and kimchi [N.B. I do not recommend these fermented foods. See Dr Greger’s video on kimichi29 , where he points out research showing that eating kimchi potentially doubles a woman’s risk of breast cancer and increases a man’s chance of getting prostate cancer by ten times – and that’s just one spoonful a day. Regarding sauerkraut, Dr Greger considers30 that the jury is out but, in my opinion, I would avoid it. Bacteria exist on cabbage without having to ferment it. Cut out the middle man and let your healthy gut bacteria do the job for you – safely!]]
- Foods rich in glycine. [Whilst also found in animal products, I recommend finding your glycine in whole plant foods such as beans; vegetables like spinach, kale, cauliflower, cabbage and pumpkin; plus fruits like banana and kiwi.]
- Probiotics [At this stage, I have to point out that probiotics are not the 100% safe option that some people would have us believe. A Dr Greger video31 makes this fact very plain. And I would recommend that, unless your doctor recommends otherwise, you always opt for the natural way of getting probiotics – by eating natural whole plant foods that provide and feed the bacteria in your gut.]
Avoiding the following:
- Antibiotics
- Indigestible or irritating foods [I do not support the idea that insoluble fibre is necessarily a bad option]
- Stress
- Getting too little sleep
The authors do state that the relationship between fibromyalgia, IBS and SIBO is still poorly understood and that more work is necessary.
Main photo from Dr Christopher Bray’s article “Fibromyalgia … A problem with the gut bacteria?”32
References
- Probiotics for fibromyalgia: study design for a pilot double-blind, randomized controlled trial. Roman P, Estévez ÁF, Sánchez-Labraca N, Cañadas F, Miras A, Cardona D. Nutr Hosp. 2017 Oct 24;34(5):1246-1251. doi: 10.20960/nh.1300. PMID: 29130724. [↩]
- Gut Microbiota & Depression [↩]
- Dinan TG, Quigley EM. Probiotics in the treatment of depression: Science or science fiction? Aust N Z J Psychiatry 2011;45(12):1023-5. [↩]
- Diaz Heijtz R, Wang S, Anuar F, Qian Y, Björkholm B, Samuelsson A, et al. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci USA 2011;108(7):3047-52. [↩]
- Hardy H, Harris J, Lyon E, Beal J, Foey AD. Probiotics, prebiotics and immunomodulation of gut mucosal defences: Homeostasis and immunopathology. Nutrients 2013;5(6):1869-912. [↩]
- Upadhyay N, Moudgal V. Probiotics: A review. J Clin Outcomes Manag 2012; 19(2):76-84. 58,59. [↩]
- Dinan TG, Stanton C, Cryan JF. Psychobiotics: A novel class of psychotropic. Biol Psychiatry 2013;74(10):720-6. [↩] [↩] [↩]
- Hardy H, Harris J, Lyon E, Beal J, Foey AD. Probiotics, prebiotics and immunomodulation of gut mucosal defences: Homeostasis and immunopathology. Nutrients 2013;5(6):1869-912. [↩]
- Desbonnet L, Garrett L, Clarke G, Bienenstock J, Dinan TG. The probiotic Bifidobacteria infantis: An assessment of potential antidepressant properties in the rat. J Psychiatr Res 2008;43(2):164-74. [↩]
- Martinowich K, Lu B. Interaction between BDNF and serotonin: Role in mood disorders. Neuropsychopharmacol 2008;33(1):73-83. [↩]
- Butt H, Dunstan R, McGregor N, Roberts T. Bacterial colonosis in patients with persistent fatigue. In: Proceedings of the AHMF international clinical and scientific conference; 2001. [↩]
- Othman M, Agüero R, Lin HC. Alterations in intestinal microbial flora and human disease. Curr Opin Gastroenterol 2008;24(1):11-6. [↩]
- Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum
1990;33(2):160-72. [↩] - Glass JM, Park DC, Minear M, Crofford LJ. Memory beliefs and function in fibromyalgia patients. J Psychosom Res 2005;58(3):263-9.)) ((Glass JM. Fibromyalgia and cognition. J Clin Psychiatry 2008;69(Suppl2):20-4. [↩]
- Glass JM. Cognitive dysfunction in fibromyalgia and chronic fatigue syndrome: New trends and future directions. Curr Rheumatol Rep 2006;8(6):425-9. [↩]
- Glass JM. Review of cognitive dysfunction in fibromyalgia: A convergence on working memory and attentional control impairments. Rheum Dis Clin North Am 2009;35(2):299-311. [↩]
- Glass JM, Williams DA, Fernández-Sánchez ML, Kairys A, Barjola P, Heitzeg MM, et al. Executive function in chronic pain patients and healthy controls: Different cortical activation during response inhibition in fibromyalgia. J Pain
2011;12(12):1219-29.14-18. [↩] - Verdejo-García A, López-Torrecillas F, Calandre EP, Delgado-Rodríguez A, Bechara A. Executive function and decision-making in women with fibromyalgia. Arch Clin Neuropsychol 2009;24(1):113-22. [↩]
- Aaron LA, Burke MM, Buchwald D. Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia, and temporomandibular disorder. Arch Intern Med 2000;160(2):221-7. [↩]
- Aaron LA, Buchwald D. A review of the evidence for overlap among unexplained
clinical conditions. Ann Intern Med 2001;134(9 Pt 2):868-81. [↩] - Buchwald D, Garrity D. Comparison of patients with chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities. Arch Intern Med 1994;
154(18):2049-53. [↩] - Francavilla R, Miniello V, Magista AM, De Canio A, Bucci N, Gagliardi F, et al. A randomized controlled trial of Lactobacillus gg in children with functional abdominal pain. Pediatrics 2010;126(6):e1445-52. [↩]
- Konieczna P, Groeger D, Ziegler M, Frei R, Ferstl R, Shanahan F, et al. Bifidobacterium infantis 35624 administration induces Foxp3 T regulatory cells in human peripheral blood: Potential role for myeloid and plasmacytoid dendritic cells. Gut 2012;61(3):354-66. [↩]
- Rao AV, Bested AC, Beaulne TM, Katzman MA, Iorio C, Berardi JM, et al. A randomized, double-blind, placebo-controlled pilot study of a probiotic in
emotional symptoms of chronic fatigue syndrome. Gut Pathog 2009;1(1):6. [↩] - Fibromyalgia and Small Intestinal Bacterial Overgrowth (SIBO). [↩]
- Hyperalgesia: ‘hyper’ from Greek (huper, “over”), ‘-algesia’ from Greek algos, (pain [↩]
- LBT: Lupus band test is a term used to describe the typical immunofluorescence microscopy findings in the skin of patients who have lupus erythematosus. [↩]
- Some fibres are readily fermented by bacteria that normally colonise the colon. In addition to increasing the amount of bacteria in the colon, fermentation results in the formation of short-chain fatty acids (acetate, propionate, and butyrate) and gases. Interestingly, the preferred energy source for colonocytes (epithelial cells that line the colon) is butyrate. Pectins, β-glucans, guar gum, inulin, and oligofructose are readily fermented, while cellulose and lignin are resistant to fermentation in the colon . Foods that are rich in fermentable fibres include oats and barley, as well as fruit and vegetables. Cereal fibres that are rich in cellulose, such as wheat bran, are relatively resistant to bacterial fermentation. [↩]
- Is Kimchi Good For You? [↩]
- Are Kimchi and Sauerkraut Harmful? [↩]
- Culture Shock – Questioning the Efficacy and Safety of Probiotics [↩]
- Fibromyalgia … A problem with the gut bacteria? [↩]