
Research in the US suggests that around one in eight people now have chronic kidney disease, mostly without even knowing about it. But why?
The answer appears to be connected with the Western-style diet (high in meat, particularly processed, and low in fruits and vegetables) which can cause:
- impairment of kidney blood flow
- inflammation
- subsequent leakage of protein in the urine
- and a rapid decrease in kidney function.
Saturated fat, trans fat, and cholesterol found in animal and junk foods negatively impact kidney function, as well.
Animal protein can deliver an acid load to the kidneys, increase ammonia production, and damage the sensitive kidney cells.
So restricting protein intake is recommended to prevent kidney function decline: “Unlimited intake of protein-rich foods, now generally regarded as ‘normal,’ may be responsible for dramatic differences in renal function between modern human beings and their remote predecessors who hunted and scavenged for meat.”
But not all protein. It’s animal protein that appears to be the problem, causing hyperfiltration, which increases the workload of the kidneys – a condition that is linked to diabetes as well as other diseases.
Diets containing an excess of animal protein – which means the diets of the majority of people living in the West – can cause unrelenting stress on our kidneys and predispose even healthy people to progressive kidney scarring and deterioration of kidney function.
One study demonstrated that, while eating meat increases the workload on the kidneys within hours of consumption, eating plant protein has no such effect. Another similar study revealed the same results with the specific consumption of beef, but any animal protein will do the same – whether organic chicken breasts or line-caught tuna fish, excess pressure on the kidneys increases within just hours of consumption. But no adverse effect occurred when tucking in to a tofu salad sandwich.
If you think you’re safe with eggs and dairy protein, think again – the harmful effects of eating these animal proteins were shown to occur in people with normal kidneys and in people with diseased kidneys.
Both short-term and long-term studies have demonstrated similar results indicating that “substituting soy protein for animal protein is associated with less hyperfiltration and [protein leakage]…therefore slowing deterioration of renal function” in the case of the former study and “the consumption of whole soy tended to preserve renal function compared with milk placebo in individuals with lowered renal function” in the case of the latter.
When diabetics were tested with soy and dairy proteins, results showed that soy protein seemed to make things better, while dairy protein made things worse.
So is it too late to change your diet once you have developed kidney disease?
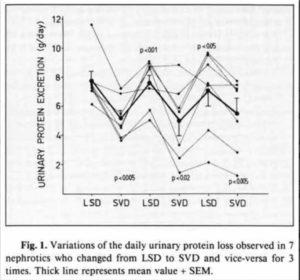
Apparently not. Even when the kidneys are so damaged that they are actively losing protein in the urine, a plant-based diet has been shown to come to the rescue. Indeed, researchers demonstrated that kidney dysfunction could be turned on and off light a light switch just by altering the diet. This remarkable fact can be seen in the following chart from the latter study. The drops are when animal protein is removed from the diet and the rises are when it’s added back in to the diet:
So why is this overloading of the kidneys happening with animal protein but not with plant protein?
It appears to be concerned with inflammation. Animal protein triggers an inflammatory response. How do we know this? Because the researchers administered a powerful anti-inflammatory drug and, hey presto! the hyperfiltration protein leakage response that occurred previously after eating meat stopped completely when the drug was administered and meat products were eaten again.
These foregoing results appear to confirm the harmful inflammatory impact on our kidneys from consuming animal protein.
So keep your kidneys on top form by keeping kidneys – and pork chops and beef burgers, for that matter – OFF the menu.

References
Ryan TP, Sloand JA, Winters PC, Corsetti JP, Fisher SG. Am J Med. 2007 Nov;120(11):981-6. Chronic kidney disease prevalence and rate of diagnosis.
Odermatt A. Am J Physiol Renal Physiol. 2011 Nov;301(5):F919-31. doi: 10.1152/ajprenal.00068.2011. Epub 2011 Aug 31.
The Western-style diet: a major risk factor for impaired kidney function and chronic kidney disease.
Soroka N, Silverberg DS, Greemland M, Birk Y, Blum M, Peer G, Iaina A. Nephron. 1998;79(2):173-80. Comparison of a vegetable-based (soya) and an animal-based low-protein diet in predialysis chronic renal failure patients.
Brenner BM, Meyer TW, Hostetter TH.. N Engl J Med. 1982 Sep 9;307(11):652-9. Dietary protein intake and the progressive nature of kidney disease: the role of hemodynamically mediated glomerular injury in the pathogenesis of progressive glomerular sclerosis in aging, renal ablation, and intrinsic renal disease.
Alexa N Sasson and David ZI Cherney. World J Diabetes. 2012 Jan 15; 3(1): 1–6. Published online 2012 Jan 15. doi: 10.4239/wjd.v3.i1.1. Renal hyperfiltration related to diabetes mellitus and obesity in human disease.
Kontessis P, Jones S, Dodds R, Trevisan R, Nosadini R, Fioretto P, Borsato M, Sacerdoti D, Viberti G. Kidney Int. 1990 Jul;38(1):136-44. Renal, metabolic and hormonal responses to ingestion of animal and vegetable proteins.
Nakamura H, Takasawa M, Kashara S, Tsuda A, Momotsu T, Ito S, Shibata A. Tohoku J Exp Med. 1989 Oct;159(2):153-62. Effects of acute protein loads of different sources on renal function of patients with diabetic nephropathy.
Chan AY, Cheng ML, Keil LC, Myers BD. J Clin Invest. 1988 Jan;81(1):245-54. Functional response of healthy and diseased glomeruli to a large, protein-rich meal.
Liu ZM, Ho SC, Chen YM, Tang N, Woo J. Clin Biochem. 2014 Sep;47(13-14):1250-6. doi: 0.1016/j.clinbiochem.2014.05.054. Epub 2014 May 27. Effect of whole soy and purified isoflavone daidzein on renal function–a 6-month randomized controlled trial in equol-producing postmenopausal women with prehypertension.
Teixeira SR, Tappenden KA, Carson L, Jones R, Prabhudesai M, Marshall WP, Erdman JW Jr. J Nutr. 2004 Aug;134(8):1874-80. Isolated soy protein consumption reduces urinary albumin excretion and improves the serum lipid profile in men with type 2 diabetes mellitus and nephropathy.
Barsotti G, Cupisti A, Morelli E, Ciardella F, Giovannetti S. Nephrol Dial Transplant. 1990;5 Suppl 1:75-7. Vegan supplemented diet in nephrotic syndrome.
Fioretto P, Trevisan R, Valerio A, Avogaro A, Borsato M, Doria A, Semplicini A, Sacerdoti D, Jones S, Bognetti E, et al. Am J Physiol. 1990 Mar;258(3 Pt 2):F675-83. Impaired renal response to a meat meal in insulin-dependent diabetes: role of glucagon and prostaglandins.