
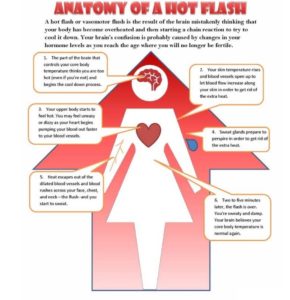
For women experiencing menopausal-related hot flushes (called hot flashes in the States), natural dietary remedies, without the side-effects 1 of the pharmaceutical alternatives, would be a pretty good option. But do such things exist? We’ll look for an answer by reviewing recent research and digesting the views of some respected doctors.
We’ll look at a variety of possible foods/plant extracts that have been researched and peer-reviewed in relation to their ability to reduce the intensity and frequency of hot flushes:
- grape seed extract
- saffron
- danggui liuhuang
- black cohosh and evening primrose oil
- red clover extract
- flaxseed (linseed)
- genistein
- soy
Blog Contents
1. Grape seed extract and hot flushes
A 2014 randomised, double-blind, placebo-controlled pilot study 2 96 women aged 40 to 60 years who had at least one menopausal symptom, were given either a low-dose or high-dose of grape seed extract tablets or a placebo for 8 weeks. Their menopausal symptoms, body composition and cardiovascular parameters were then measured after 4 and 8 weeks.
Study results
The following significant changes were observed in the high-dose group after 8 weeks:
- physical symptoms improved
- hot flushes reduced
- insomnia decreased
- anxiety and depression reduced
- systolic and diastolic blood pressure decreased (in both low- and high-dose groups after 4 weeks)
- muscle mass increased (in both low- and high-dose groups after 8 weeks)
These were pretty impressive results by any standards. The researchers concluded: “Grape seed proanthocyanidin 3 extract is effective in improving the physical and psychological symptoms of menopause while increasing muscle mass and reducing blood pressure in middle-aged women.”
This is the only research I’ve come across on grape seed proanthocyanidin extract and hot flushes. A letter written by Dr Kadri Altundag made the following comment 4 on this research study: “In this randomized, doubleblind, placebo-controlled study, women taking grape seed extract with concentrated amounts of the polyphenol antioxidant proanthocyanidin showed improved menopausal symptoms (including hot flashes, anxiety, and insomnia). However, more studies are needed to confirm its use as an alternative treatment for hormone therapy–related hot flashes.”
2. Saffron
A 2018 double-blind, randomised, placebo-controlled trial 5 expressed concerns about the side-effects of hormone therapy, and thus looked at the efficacy and safety of saffron (stigma of Crocus sativus) in treatment of major depressive disorder associated with post-menopausal hot flashes.

Sixty women with post-menopausal hot flushes were randomly selected to receive either saffron (30 mg/day, 15 mg twice per day) or a placebo for a period of 6 weeks. Hot flush and depression ratings were taken at baseline and at the second, fourth, and sixth weeks of the study.
Study results
This study revealed that saffron is a safe and effective treatment in improving hot flushes and depressive symptoms in post-menopausal healthy women. The researchers added: “…saffron, with fewer side effects, may provide a non-hormonal and alternative herbal medicine option in treatment of women with hot flashes.”
As far as I can see, there are no other research studies on saffron and hot flushes. However, there are studies on other effects of saffron in animal and human studies. One such study concluded that: “…aqueous and ethanolic ((Definition of ethanolic: of, pertaining to, containing, producing or using ethanol.)) extracts of saffron stigma and petal have an antinociceptive ((Definition of antinociceptive: nociception is the sensory nervous system’s response to certain harmful or potentially harmful stimuli. Antinociception is the action or process of blocking the detection of a painful or injurious stimulus by sensory neurons.)) effect, as well as acute and/or chronic anti-inflammatory activity.”
3. Danggui Liuhuang
Danggui Liuhuang (DLH) decoction 6 is a traditional herbal medicine widely used in East Asia to treat menopausal symptoms.

Herbal medicine is widely used in East Asian countries such as Korea, China, and Japan. The use of these is likely to increase because of the side-effects of traditional hormone replacement therapy (HRT) 7 8 . Danggui Liuhuang decoction in Korea and China has been prescribed for the treatment for night sweats, fever, red face, distress, dry mouth, and constipation. DLH decoction consists of 7 medicinal herbs:
- Angelicae Gigantis Radix
- Astragali Radix
- Coptidis Rhizoma
- Rehmanniae Radix Crudus
- Rehmanniae Radix Preparata
- Phellodendri Cortex, and
- Scutellariae Radix 9 10
Studies appear to show that DLH decoction has immunomodulatory 11 and anti-inflammatory effects 12 . Although I can’t get hold of any studies on its relationship to hot flushes, a systematic review 13 is currently planned that will summarise and critically assess evidence from randomised controlled trials that have investigated the use of DLH decoction for the treatment of menopausal symptoms.
4. Black cohosh and evening primrose oil
A 2018 comparative study 14 compared the efficacy of black cohosh (cimicifuga racemosa, also known as black bugbane, back snakeroot, fairy candle) 15 and evening primrose oil (EPO) in postmenopausal women with menopause-related symptoms.

Both of these are easily available at health food stores, etc.

This study was performed on 80 postmenopausal women with hot flashes. The participants were randomly divided into two groups: one group received black cohosh and the other group received EPO for 8 weeks. The severity and number of hot flushes and quality of life were measured and analysed.
Study results
At the end of the study:
- average severity of hot flushes in both groups were significantly lower
- number of hot flushes in black cohosh group were significantly lower
- number of hot flushes in EPO group were not significantly lower
The researchers concluded: “Both herbs were effective in reduction of severity of hot flashes and improvement of the quality of life, but it seems that black cohosh is more effective than primrose oil because it was able to reduce the number of hot flashes too.”
A 2009 randomised controlled trial 16 found that compared with placebo, black cohosh did not reduce the number of vasomotor (hot flush) symptoms.
There are, however, conflicting reports about the safety of black cohosh for menopausal symptoms. The latter study 16 concluded: “Safety monitoring indicated that chemically and biologically standardized extracts of black cohosh…were safe during daily administration for 12 months.” A July 2008 study 17 concluded: “The efficacy of black cohosh as a treatment for menopausal symptoms is uncertain and further rigorous trials seem warranted.” A further November 2008 study 18 concluded: “…black cohosh has been associated with serious safety concerns that urgently require further investigation.” On the other hand, a 2018 study 19 pointed out some positive results of its use with no side effects in subjects at the end of the 12th month of monitoring. It does, however, also mention cases of liver damage as a result of its use.
In relation to evening primrose oil, there are some reports 20 of mild side-effects (such as headache and stomach upset) as well as negative interactions when individuals are taking anticoagulant, antiplatelet, anti-schizophrenia, or anti-psychotic medications 21 . It was once associated with epileptic seizures, but a 2007 study 22 concluded that there never was no such association and the earlier studies implying an association were flawed.
5. Red clover extract
A 2014 meta-analysis 23 looked at published data on red clover extract (RCE) being used for the alleviation of hot flushes in postmenopausal women and concluded: “The safety and efficacy of red clover for alleviating menopausal hot flushes are yet to be established…red clover when compared to placebo was effective in reducing menopausal hot flushes when administered for 3-4 months , but their effect did not persist at 12 months.”

There are conflicting reports on both the safety and efficacy of RCE in the treatment of hot flushes. A 2017 parallel, double blind, randomised control trial 24 concluded: “Results suggest that moderate doses of RCE were more effective and superior to placebo in reducing physiological and self-reported VMS [vasomotor symptoms, i.e. hot flushes]. Findings support that objective physiological symptom assessment methods should be used together with self-report measures in future studies on menopausal VMS.” A 2013 systematic review 25 found that, while evidence on the safety and efficacy of red clover is limited, at least there did not appear to be any breast cancer-promoting effects associated with its use. A 2009 study 16 mentioned earlier concluded: “Compared with placebo…red clover did not reduce the number of vasomotor symptoms. Safety monitoring indicated that chemically and biologically standardized extracts of … red clover were safe during daily administration for 12 months.”
An article on WebMD 26 lists some pretty serious side-effects of red clover extract for pregnant or breast-feeding women, as well as some side-effects of which other people should be aware. It’s worth quoting some of the article:
“Red clover is LIKELY SAFE for most people when used in the amounts found in food…It is POSSIBLY SAFE when used in medicinal amounts by mouth or applied to the skin….Red clover can cause rash-like reactions, muscle ache, headache, nausea, and vaginal bleeding (spotting) in some women. Bleeding disorders: Red clover might increase the chance of bleeding. Avoid large amounts and use with caution. Hormone-sensitive conditions such as breast cancer, uterine cancer, ovarian cancer, endometriosis, or uterine fibroids: Red clover might act like estrogen. If you have any condition that might be made worse by exposure to estrogen, don’t use red clover. Protein S deficiency: People with protein S deficiency have an increased risk of forming blood clots. There is some concern that red clover might increase the risk of clot formation in these people because it has some of the effects of estrogen. Don’t use red clover if you have protein S deficiency. Surgery: Red clover might slow blood clotting. It might increase the chance of extra bleeding during and after surgery. Stop taking red clover at least 2 weeks before a scheduled surgery. There isn’t enough information to rate the safety of red clover when applied to the skin.”
6. Flaxseed
There are very few studies into the possible benefits of flaxseed for treating hot flushes. However, a 2016 systematic review and meta-analysis 27 found that flaxseed showed beneficial effect on hot flush frequency and intensity, although not statistically significant. However, they concluded: “The results of our systematic review suggest beneficial effect on vasomotor symptom with…flaxseed…Further trials are still needed to confirm the results of our systematic review.”

The latter study also looked at the effect of hypericum perforatum (St John’s-wort) and vitex agnus-castus (lilac, also called vitex, chaste tree, chasteberry, Abraham’s balm, lilac chastetree, or monk’s pepper) and found that they had a similarly positive effect to flaxseed in reducing frequency and intensity of hot flushes.

However, because of concerns about side-effects and potentially dangerous interactions of St John’s-wort 28 and vitex agnus-castus 29 , I am not going to recommend them at all.
7. Genistein
Genistein is an isoflavone 30 that is described as an angiogenesis inhibitor and a phytoestrogen. It was first isolated in 1899 from the dyer’s broom, genista tinctoria, and hence its chemical name. It’s also found in soybeans, lupins, fava beans, etc. Isolating the phytoestrogen genistein from the whole food makes money for pharmaceutical companies, whilst simply eating the whole food itself does not. And whilst I would always suggest the latter wholefood approach, there’s some research on the former “tablet-based” approach which is probably worth mentioning in passing.
A 2009 2-year randomised, double-blind, placebo-controlled study 31 split 389 subjects into genistein and placebo groups. They were testing mainly for reductions from the baseline in the frequency and severity of hot flushes.
Study results
- after 12 months of genistein therapy, there was a significant reduction (-56.4%) in the mean number of hot flushes, with a significant difference compared with the control group
- after 24 months, there was no further decrease in the number of hot flushes in both groups
They concluded: “The phytoestrogen genistein has been shown to be effective on vasomotor symptoms without an adverse effect on the endometrium and vagina, but after the first year, there was no further improvement in the decrease in hot flushes.”
A 2011 12-week randomised double-blind, placebo-controlled study 32 evaluated the efficacy of synthetic genistein for reducing the frequency and severity of hot flushes in 84 postmenopausal women. They concluded: “The current study provides the first evidence that a single daily dose of 30 mg of synthetic genistein reduces hot flush frequency and duration.”
Rather than spend time looking at the isolated isoflavone, we’ll concentrate on soy as the natural whole food source.
8. Soy
There’s plenty of research on the safety and efficacy of soy in relation to hot flushes and postmenopausal symptoms in general. Additionally, there’s been lots of debate over the years about the safety of soy in relation to IGF-1 (a cancer-promoting growth hormone involved in the acquisition and progression of malignant human tumours). In order to form an opinion about soy, it would be useful to consult with both Dr Greger and Dr McDougall.

Dr Greger’s view on soy and the menopause
In an usually short and punchy video 33 , Dr Greger comments on the fact that there’s mixed results from research, but he has no doubt that soy consumption does help ameliorate symptoms of menopause. He refers to a 2008 review34 which looked at 12 previous studies into this topic. You will see from the chart below that, while one study showed an increase in hot flushes, and three showed no significant change, 8 of the studies showed a significant decrease in the number of hot flushes. The reviewers concluded: “Consumption of 30 mg/day of soy isoflavones…reduces hot flashes by up to 50 %. This total reduction includes that provided by “the placebo effect”. The greatest benefit may be realized when the isoflavone-rich food…is taken in divided doses by subjects who experience at least four hot flashes/day.”
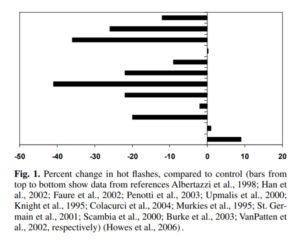
Dr Greger ends his video by saying: “You can imagine what the headlines were like after the publication of that last study. “Soy doesn’t work!” But you have to take the totality of evidence, and overall, soy really does seem to help.”
Dr McDougall’s view on soy and the menopause
Within the context of a very detailed article 35 on the possible benefits and risks of soy consumption, Dr McDougall looks at the detrimental and beneficial effects of soy on female sex hormones:
“Detrimental: Twelve ounces of soy milk drunk three times a day for one month will decrease a woman’s estradiol 36 and progesterone levels, and her menstrual cycle length will be increased by about four days 37 . These effects may cause infertility and contribute to bone loss.
Beneficial: Chinese and Japanese are among the most prolific baby-makers in the world. Phytoestrogens have both a weak estrogen-stimulating (estrogenic) and paradoxically, an estrogen-inhibiting (anti-estrogenic) activity. The estrogen-like activities may strengthen bones and prevent menopausal symptoms like hot flashes. Hot flashes are reported 38 by 70% to 80% of US menopausal women compared to 10 to 14% of women in Japan and Singapore. The anti-estrogen activity reduces the risk of breast and uterine cancer.”
He makes the following recommendations on the amount and type of soy products we should consume:
- use traditional soy foods, like soy milk and tofu, only as a small part of your diet, at most 5% of your daily calories
- “Synthetic soy foods,” like meats, cheeses, and soy bars, should rarely, if ever, be consumed
- sensible uses of soy might be:
- unsweetened soy milk (ideally organic) to moisten cereal, not glassfuls as a beverage
- tofu pieces in a “stir-fry” rice dish, not as a soy burger entrée
- occasional tofu-based dessert, not daily soy “candy” bars
Whilst he doesn’t mention edamame (the delicious immature soybeans taken from the pod – whether fresh or from frozen), they are an excellent way of consuming soy, especially in salads.

Some research on soy and hot flushes
A randomised, double-blind, placebo-controlled 2007 study 39 split 80 women (mean age = 55.1 years), who reported 5 or more hot flush episodes per day, into two groups: one group received 250 mg of standardised soy extract and the other group received a placebo. They were then followed for 10 months and assessed. The results showed that at the end of the period, there was a significant reduction in frequency of hot flushes among isoflavone users when compared to those on placebo. No serious adverse event related to isoflavone treatment was reported. They concluded: “The soy isoflavone extract exerted favorable effects on vasomotor symptoms and good compliance, providing a safe and effective alternative therapeutic for postmenopausal women.”
A 2015 meta-analysis 40 reviewed 16 studies on soy isoflavones and found found that the maximal percentage change of hot flashes reduction by soy isoflavones was 25.2% after elimination of the placebo effect. They found that it was about half as effective as the drug Estradiol 41 , which can have some pretty nasty side-effects 42 . Additionally, a time interval of 13.4 weeks was needed for soy isoflavones to achieve half of Estradiol’s maximal effects, while estradiol only required 3.09 weeks to start having an effect. The results suggest that treatment intervals of 12 weeks are too short for soy isoflavones, which require at least 48 weeks to achieve 80% of their maximum effects. They concluded: “Soy isoflavones show slight and slow effects in attenuating menopausal hot flashes compared with estradiol.”
A 2014 editorial article 43 on the effectiveness of soybeans being used to treat hot flushes, concluded: “…the overwhelming amount of evidence indicates that isoflavone supplements, provided they contain a sufficient amount of genistein, alleviate hot flashes to a clinically relevant extent and have an acceptable safety profile. The amount of total isoflavones (expressed in aglycone equivalent weight) needed for relief is estimated to be approximately 40–50 mg/day, which is provided by approximately two servings of traditional soyfoods, an amount that is well within the range of the soy/isoflavone intake of older adults in Japan 44 . Therefore, health professionals and clinicians are justified in advising their clients and patients to try isoflavones for the relief of hot flashes.”
A 2018 placebo-controlled double-blind trial 45 assessed the potency of a soy germ preparation for the alleviation of menopausal hot flushes in 180 participants. Soy germ extract (100 mg of the soy isoflavone glycoside) was given.
The results after 12 weeks of double-blind treatment showed an improvement in the soy consuming group of 71% in terms of reduced hot flushes, and 78% in terms of sweating. They concluded: “Soy germ extract with 100 mg of isoflavone glycosides was shown to modestly, but significantly reduce menopausal hot flushes.”
Of course, the limited 12-week period of this latter study could not evaluate long-term effects of soy consumption.
Joe’s comments
There doesn’t seem to be enough research on grape seed extract to justify any strong claims about its efficacy for treating menopausal issues, including hot flushes; although the impressive results achieved, combined with the lack of any evidence of side-effects or negative interactions with other foods, would probably justify inclusion of it within a dietary plan.
Only one study appears to deal with saffron and hot flushes. The results seemed positive and without side-effects or negative interactions with other foods. However, saffron is pretty expensive ($3000/£2600 per kilo 2018 prices 46 and cheaper alternatives might be preferable. Of course, because of the other health benefits it possesses, if you can afford to include it in your daily food plan, why not?!
Although danggui liuhuang (DLH) decoction has been used for a long time in Asia for the treatment of a variety of conditions, there’s insufficient research data to draw any conclusions about its effectiveness in relation to hot flushes. It may be wise to stay away from it – even if you could find a supplier – until further research has been published.
There’s sufficient doubt about black cohosh to justify caution, whilst taking evening primrose oil (probably best after consultation with a doctor) appears less potentially problematic and has been demonstrated to reduce the severity of hot flushes.
The potential of side-effects with red clover extract would suggest that it should only be used with caution and certainly only after consultation with a doctor.
Flaxseed (also called linseed) is such an amazing food, with astounding health benefits 47 , that I recommend consuming at least a tablespoon of ground flaxseeds every day. Its potential for reducing intensity and frequency of hot flushes would would be an added benefit.
I would suggest that taking isolated genistein is again only something that should be considered after medical consultation. There are always going to be concerns about extracting bits out of a whole food, concentrating them in a potion and then expecting the body to metabolise them effectively without any side-effects. The same could be said about all the other extracted substances listed above.
There appear to be clear benefits of consuming soy as a means of cooling the heat of menopausal-related hot flushes. Soy also has also been shown to have many other benefits (such as lowering LDL cholesterol 48 49 50 and postprandial triglyceride levels 51 , not covered in this blog, but covered in great detail 52 by Dr Greger in articles and videos. As a small part of a well-balanced diet, soy in its various non-highly-processed forms seems well worth trying, although any benefits are not likely to appear until after several weeks or even months after regular daily consumption.
There are a number of other ‘natural’ remedies you might like to research but which are not covered in this blog:
- sage
- camomile
- green tea
- thyme tea and other herbal teas (melisse, cinnamon, ginger, mallow, lavender, carnation, rosemary, fennel, lemon balm, French lavender, okra flower, nettle)
- apple cider vinegar
Additionally, a few other more general suggestions for reducing hot flushes do deserve a final mention:
- reduce animal protein intake (so-called “meat sweats” are worth looking into)
- include some foods rich in vitamin E in your diet (nuts, seeds, avocado, etc but not as a vitamin supplement 53 )
- reduce/eliminate toxins from your body (ideally achieved by water fasting 54 and/or eating a non-SOS WFPB diet)
- stay well-hydrated (drink at least 1.5-2 litres of water a day)
- exercise regularly 55 )
- reduce stress with mindfulness techniques 56
References
- JAMA. 2002 Jul 17;288(3):321-33. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial.
Rossouw JE1, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J; Writing Group for the Women’s Health Initiative Investigators. [↩] - Effects of grape seed proanthocyanidin extract on menopausal symptoms, body composition, and cardiovascular parameters in middle-aged women: a randomized, double-blind, placebo-controlled pilot study. Terauchi, Masakazu MD, PhD, NCMP; Horiguchi, Noe BS; Kajiyama, Asuka MD; Akiyoshi, Mihoko PhD; Owa, Yoko BS; Kato, Kiyoko BS; Kubota, Toshiro MD, PhD. Menopause: September 2014 – Volume 21 – Issue 9 – p 990–996. [↩]
- Definition of proanthocyanidins: Proanthocyanidins are also known as condensed tannins and are very powerful antioxidants that remove harmful free oxygen radicals from cells. They are a class of polyphenols found in a variety of plants. Chemically, they are oligomeric flavonoids. [↩]
- Could Grape Seed Extract Be an Alternative Treatment in the Management of Hot Flashes? by Dr Kadri Altundag [↩]
- Arch Gynecol Obstet. 2018 Mar;297(3):717-724. Efficacy of Crocus sativus (saffron) in treatment of major depressive disorder associated with post-menopausal hot flashes: a double-blind, randomized, placebo-controlled trial. Kashani L, Esalatmanesh S, Eftekhari F, Salimi S, Foroughifar T, Etesam F, Safiaghdam H, Moazen-Zadeh E, Akhondzadeh S. [↩]
- Definition of decoction: a concentrated liquor resulting from heating or boiling a substance, especially a medicinal preparation made from a plant. [↩]
- Posadzki P, Lee MS, Moon TW, et al. Prevalence of complementary and alternative medicine (CAM) use by menopausal women: a systematic review of surveys. Maturitas 2013;75:34–43. [↩]
- Xu LW, Jia M, Salchow R, et al. Efficacy and side effects of Chinese herbal medicine for menopausal symptoms: a critical review. Evid Based Complement Alternat Med 2012;2012:568106. [↩]
- Yeogang Publishing Company, Hur J. Dongui Bogam. 2005;Originally published in 1610. [↩]
- Li DY. Lan Shi Mi Cang. 2012;China: China Tianjin Science and Technology Press, Originally published in 1276. [↩]
- Kim DG, Kim KS. Effects of dangkwiyughwangtang and okbyoungpoongsangamibang on the immune response induced by methotrexate in mice. J Korean Orient Pediatr 2007;21:189–209. [↩]
- Kim SB, Kang OH, Keum JH, et al. Anti-inflammatory effects of Danggui Liuhuang Decoction () in RAW 264.7 cells. Chin J Integr Med 2012;1–7. [↩]
- Medicine (Baltimore). 2018 Jan; 97(4): e9735. Herbal medicine (Danggui Liuhuang decoction) for managing menopausal symptoms. A protocol of systematic review of randomized clinical trials. Ji Hee Jun, MSc, Hye Won Lee, PhD, Junhua Zhang, MD PhD, Fengwen Yang, MD PhD, and Myeong Soo Lee, PhD. [↩]
- J Educ Health Promot. 2018; 7: 36. A comparative study on the effect of “black cohosh” and “evening primrose oil” on menopausal hot flashes. Maryam Mehrpooya, Soghra Rabiee, Amir Larki-Harchegani, Amir-Mohammad Fallahian, Abbas Moradi, Sara Ataei, and Masoumeh Taravati Javad. [↩]
- More info on black cohosh [↩]
- Menopause. 2009 Nov-Dec;16(6):1156-66. Safety and efficacy of black cohosh and red clover for the management of vasomotor symptoms: a randomized controlled trial. Geller SE, Shulman LP, van Breemen RB, Banuvar S, Zhou Y, Epstein G, Hedayat S, Nikolic D, Krause EC, Piersen CE, Bolton JL, Pauli GF, Farnsworth NR. [↩] [↩] [↩]
- Pharmacol Res. 2008 Jul;58(1):8-14. doi: 10.1016/j.phrs.2008.05.008. Epub 2008 Jun 8. Black cohosh (Cimicifuga racemosa) for menopausal symptoms: a systematic review of its efficacy. Borrelli F, Ernst E. [↩]
- Am J Obstet Gynecol. 2008 Nov;199(5):455-66. Black cohosh (Cimicifuga racemosa): a systematic review of adverse events. Borrelli F, Ernst E. [↩]
- Black Cohosh (Actaea Racemosa, Black Bugbane, Black Snakeroot, Fairy Candle). Randy W. Wobser; Mark V. Pellegrini. Creighton University School of Medicine. Last Update: January 31, 2018. [↩]
- Am Fam Physician. 2009 Dec 15;80(12):1405-8. Evening primrose oil. Bayles B, Usatine R. [↩]
- WebMD: Evening Primrose Oil. [↩]
- Prostaglandins Leukot Essent Fatty Acids. 2007 Aug;77(2):101-3. Epub 2007 Aug 30. The safety of evening primrose oil in epilepsy. Puri BK. [↩]
- Maturitas. 2014 Sep;79(1):58-64. doi: 10.1016/j.maturitas.2014.06.018. Epub 2014 Jul 10. Red clover extract for alleviating hot flushes in postmenopausal women: a meta-analysis. Gartoulla P, Han MM. [↩]
- PLoS One. 2017 Jun 7;12(6):e0176590. doi: 10.1371/journal.pone.0176590. eCollection 2017. Combined Red Clover isoflavones and probiotics potently reduce menopausal vasomotor symptoms. Lambert MNT, Thorup AC, Hansen ESS2, Jeppesen PB. [↩]
- PLoS One. 2013 Nov 28;8(11):e81968. doi: 10.1371/journal.pone.0081968. eCollection 2013. Soy, red clover, and isoflavones and breast cancer: a systematic review. Fritz H, Seely D, Flower G, Skidmore B, Fernandes R, Vadeboncoeur S, Kennedy D, Cooley K, Wong R, Sagar S, Sabri E, Fergusson D. [↩]
- WebMD. Red Clover: Side effects and safety [↩]
- Avicenna J Phytomed. 2016 May-Jun; 6(3): 273–283. Effects of flaxseed and Hypericum perforatum on hot flash, vaginal atrophy and estrogen-dependent cancers in menopausal women: a systematic review and meta-analysis. Masumeh Ghazanfarpour, Ramin Sadeghi, Robab Latifnejad Roudsari, Talat Khadivzadeh, Imaneh khorsand,5Maliheh Afiat, and Mahdi Esmaeilizadeh. [↩]
- Healthline: St. John’s Wort: The Benefits and the Dangers [↩]
- WebMD: Side -effects of vitex agnus-castus [↩]
- Definition of isoflavones: Isoflavones are a class of phytochemicals, which are compounds found only in plants (phyto means plant). They are also a type of phytoestrogen, or plant hormone, that resembles human oestrogen in chemical structure yet are weaker. [↩]
- Menopause. 2009 Mar-Apr;16(2):301-6. doi: 10.1097/gme.0b013e318186d7e2. Effects of the phytoestrogen genistein on hot flushes, endometrium, and vaginal epithelium in postmenopausal women: a 2-year randomized, double-blind, placebo-controlled study. D’Anna R1, Cannata ML, Marini H, Atteritano M, Cancellieri F, Corrado F, Triolo O, Rizzo P, Russo S, Gaudio A, Frisina N, Bitto A, Polito F, Minutoli L, Altavilla D, Adamo EB, Squadrito F. [↩]
- Maturitas. 2011 Feb;68(2):189-96. doi: 10.1016/j.maturitas.2010.11.012. Epub 2010 Dec 15. The effect of synthetic genistein on menopause symptom management in healthy postmenopausal women: a multi-center, randomized, placebo-controlled study. Evans M, Elliott JG, Sharma P, Berman R, Guthrie N. [↩]
- Soy Foods & Menopause. Michael Greger M.D. FACLM December 25th, 2009 Volume 3. [↩]
- Inflammopharmacology. 2008 Oct;16(5):227-9. doi: 10.1007/s10787-008-8021-z. Soy consumption for reduction of menopausal symptoms. Kurzer MS. [↩]
- The McDougall Newsletter Vol.4 No.4. Soy – Food, Wonder Drug, or Poison? [↩]
- Definition of estradiol: also spelled oestradiol, is an oestrogen steroid hormone and the major female sex hormone. It is involved in the regulation of the oestrous and menstrual female reproductive cycles. [↩]
- Cancer Epidemiol Biomarkers Prev. 1996 Jan;5(1):63-70.
Effects of soya consumption for one month on steroid hormones in premenopausal women: implications for breast cancer risk reduction. Lu LJ, Anderson KE, Grady JJ, Nagamani M. [↩] - Arch Intern Med. 2001 May 14;161(9):1161-72. A review of the evidence for the use of phytoestrogens as a replacement for traditional estrogen replacement therapy. Glazier MG, Bowman MA. [↩]
- Maturitas. 2007 Nov 20;58(3):249-58. Epub 2007 Oct 29. Efficacy and safety of a soy isoflavone extract in postmenopausal women: a randomized, double-blind, and placebo-controlled study. Nahas EA, Nahas-Neto J, Orsatti FL, Carvalho EP, Oliveira ML, Dias R. [↩]
- Br J Clin Pharmacol. 2015 Apr;79(4):593-604. doi: 10.1111/bcp.12533. Quantitative efficacy of soy isoflavones on menopausal hot flashes. Li L1, Lv Y, Xu L, Zheng Q. [↩]
- Nice: Estradiol as a drug. [↩]
- Nice: Estradiol side-effects. [↩]
- Womens Health (Lond). 2014 Nov;10(6):549-53. doi: 10.2217/whe.14.38.
Soybean isoflavones warrant greater consideration as a treatment for the alleviation of menopausal hot flashes.
Messina M. [↩] - Nutr Cancer. 2006;55(1):1-12. Estimated Asian adult soy protein and isoflavone intakes. Messina M, Nagata C, Wu AH. [↩]
- Soy germ extract alleviates menopausal hot flushes: placebo-controlled double-blind trial. Article (PDF Available) in European journal of clinical nutrition 72(S1):1 · May 2018. DOI: 10.1038/s41430-018-0173-3. [↩]
- Golden Saffron: Saffron Price in 2018 [↩]
- nutritionfacts: Flax seeds [↩]
- Zhan, Siyan; Ho, Suzanne C. (December 2005). “Meta-Analysis of the Effects of Soy Protein Containing Isoflavones on the Lipid Profile”. American Journal of Clinical Nutrition (American Society for Nutrition) 81 (2): 397–408. PMID 15699227. [↩]
- Harland, J. I.; Haffner, T. A. (September 2008). “Systematic Review, Meta-analysis and Regression of Randomised Controlled Trials Reporting an Association Between an Intake of Circa 25 g Soya Protein Per Day and Blood Cholesterol”. Atherosclerosis (European Atherosclerosis Society) 200 (1): 13–27. doi:10.1016/j.atherosclerosis.2008.04.006. PMID 18534601. [↩]
- Reynolds, K.; Chin, A.; Lees, K. A.; Nguyen, A.; Bujnowski, D.; He, J. (September 2006). “A Meta-analysis of the Effect of Soy Protein Supplementation on Serum Lipids”. The American Journal of Cardiology (American College of Cardiology.) 98 (5): 633–40. doi:10.1016/j.amjcard.2006.03.042. PMID 16923451. [↩]
- Santo, Antonio S.; Santo, Ariana M.; Browne, Richard W.; Burton, Harold; Leddy, John J.; Horvath, Steven M.; Horvath, Peter J. (December 2010). “Postprandial Lipemia Detects the Effect of Soy Protein on Cardiovascular Disease Risk Compared with the Fasting Lipid Profile”. Lipids (American Oil Chemists’ Society) 45 (12): 1127–1138. doi:10.1007/s11745-010-3487-z. PMID 20981505. [↩]
- nutritionfacts: soy [↩]
- Dangers of Vitamin E supplementation: Wong VCK, Lim CED, Luo X, Wong WSF. Current alternative and complementary therapies used in menopause. Gynecol Endocrinol. 2009;25:166–74. [↩]
- Fuhrman, Dr. Joel. Fasting and Eating for Health: A Medical Doctor’s Program For Conquering Disease. [↩]
- Menopause. 2014 Apr; 21(4): 330–338. PMID: 23899828. Efficacy of Exercise for Menopausal Symptoms: A Randomized Controlled Trial. Barbara Sternfeld et al. [↩]
- Menopause. 2011 Jun; 18(6): 611–620. PMID: 21372745. Mindfulness Training for Coping with Hot Flashes: Results of a Randomized Trial. James Carmody, Ph.D., Associate Professor of Medicine,corresponding author Sybil Crawford, Ph.D., Professor of Medicine, Elena Salmoirago-Blotcher, M.D., Doctoral Fellow, Katherine Leung, MPH, Biostatistician, Linda Churchill, M.S., Project Director, and Nicholas Olendzki, B.A., Research Coordinator. [↩]
