Dr Greger just published a video 1 (see end of blog) in which he considers whether marijuana could be of benefit to public health as well as the public purse (government spending on healthcare – specifically painkillers). The research he mentions is so interesting that I thought you might be interested in a brief synopsis of the main points raised.
Blog Contents
Widescale opioid painkiller addiction?
Research 2 shows that in the USA, more than 200 million opioid painkiller prescriptions are written every year – ”a number closely approximating the entire adult population.” Pretty shocking, don’t you think? This is not just a statistical matter – over 2.5 million Americans are addicted to them and, what’s even more shocking, more than 80 Americans die each year of overdose from these legally prescribed painkillers.
Gateway drugs
It’s quite common for people to think that marijuana is a gateway drug to stronger drugs like heroin. But not so many realise that the above research shows it’s prescription painkillers that more commonly acts as the gateway to hard drug addiction.
The financial cost
The financial cost of these painkillers (ignoring the knock-on costs in terms of the lost earning potential and also the subsequent health costs as people drift into heavy drug addiction) is US$78 million a year.
Marijuana as a gateway drug
If people are getting so addicted to painkillers, and these legally-prescribed drugs are seem to lead to harder addictions, then shouldn’t governments be even more determined to stop any possibility of marijuana being legalised (or used) as a means of controlling pain? This is certainly the opinion of many people – including the White House Spokesperson Sean Spicer, who said: “the last thing we should be doing is encouraging people” to smoke cannabis. But is marijuana really a gateway drug? And, if so, is it any better or worse than prescription painkillers? First, I suppose we need to know whether marijuana is an effective painkiller.
Is marijuana effective as a painkiller?
Research 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 going back over decades does seem to indicate that compounds (such as THC) 18 within marijuana (or whole marijuana weed) can indeed be used as an effective painkiller for a wide range of medical conditions – from migraines to cancer, MS to spinal cord injuries. Information on such research has been written about for decades, including a well-known book published in November 2000 by Alison Mack 19 .
Is marijuana a workable alternative to opioids?
A more recent 2014 study 20 stated that if there was increased access to medical cannabis, they it may: “…reduce opioid analgesic use by patients with chronic pain, and therefore reduce opioid analgesic overdoses.” And they conclude by confirming that, in the USA: “Medical cannabis laws are associated with significantly lower state-level opioid overdose mortality rates.” This consequential reduction in opiates was supported by addition research in 2017 21 , which also saw its use being responsible for a reduction in patients’ need for other medications, including those for depression, anxiety, migraines, insomnia, and even being responsible for reducing alcohol consumption. It was even found 22 to be effective in reducing the amount of crack cocaine used by addicts!
Furthermore, there’s a real problem with large amounts of opiates being used to control pain, particularly for end of life cancer patients. They get so doped-out that they cannot even communicate with their loved ones. This was highlighted in a 2016 study 23 , with the researchers stating that: “Patients who have been put on high doses of opiates at the end of life by their well-meaning oncologist or palliative care team frequently feel totally unable to communicate with their loved ones in their precious remaining time because of altered cognition.” As a potential solution to this, the researchers continue: “Many have successfully weaned themselves down or off their opiate dose by adding cannabis to their regime.” They point out that: “Cannabis species have been used as medicine for thousands of years; only since the 1940s has the plant not been widely available for medical use.”
They then provide a list of additional medical conditions for which marijuana may be considered a useful treatment:
- anorexia
- chemotherapy-induced nausea and vomiting
- pain
- insomnia
- depression
They go on to state that cannabinoids 24 have a possible direct anticancer effect by way of a number of different mechanisms involving apoptosis (cell death), angiogenesis 25 , and the inhibition of metastasis 26 . They do point out, in this case, that there are insufficient clinical trials to prove or disprove the: “…abundant anecdotal reports that describe patients having remarkable responses to cannabis as an anticancer agent, especially when taken as a high-potency orally ingested concentrate…”
Current disconnect between US official position & research findings
Of course, we know it’s widely argued by legislators in many countries that legalising marijuana for medical use might lead to more addiction (to opioid painkillers and/or harder drugs) and hence more overdose-related deaths. And, so we see that in spite of the scientific evidence, on the one hand, for the problems associated with legally sanctioned opioid drugs and, on the other hand, for its medical effectiveness (just some evidence of which is mentioned above), the current official position of the AMA (American Medical Association) 27 , like so many national government medical bodies, is that marijuana: “has no scientifically proven, currently accepted medical use for preventing or treating any disease.” But, I think we should be careful about assuming that what is said by the AMA etc and what is revealed by scientific research are one and the same thing. I suggest that the above-mentioned research indicates a discrepancy between the official line and the facts revealed through scientific studies. This is in spite of the conclusions from research 20 undertaken in those US states which legalised the medical use of marijuana between 1999 and 2010. The researchers of this study concluded that: “Medical cannabis laws are associated with significantly lower state-level opioid overdose mortality rates.” That is, all you need to do to reduce the number of deaths associated with opioid overdose is to legalise the use of medical marijuana. This was reinforced by another study 28 around the same time which confirmed that: “…medical cannabis laws were associated with a mean 24.8% lower annual rate of opioid analgesic deaths…compared with states without laws…If true, this finding upsets [not only] the applecart of conventional wisdom regarding the public health implications of marijuana legalization [but also of its] medicinal usefulness.”
The evidence for the benefits of legalising medical marijuana use doesn’t stop there. A 2016 study 29 indicated that the demand for other non-painkiller prescription drugs dropped significantly once medical marijuana was legalised – including anti-anxiety drugs, antidepressants, anti-nausea drugs, antipsychotics, anti-seizure drugs, and sleeping pills. The researchers pointed out that if all US states did this, then it could save almost US$500 million a year.
Why do governments ignore the research?
But if there is such a disconnect between official statements aimed at informing public opinion and the actual scientific evidence, who does this benefit?
Just think about it. If the 2016 study just mentioned above found that taxpayers could save themselves almost half a billion dollars a year in pharmaceutical bills, then who suffers? Big Pharma, of course. There’s no coincidence in the documented fact 30 that pharmaceutical companies (as well as the beer industry and, revealingly, the police unions and private prison industry!) were major sponsors of marijuana prohibition. This is really no different from what we see on a regular basis within the field of nutrition, where the likes of McDonald’s and Coca-Cola sponsor studies that support supposed health benefits of their products, while they marginalise or try to debunk the bulk of valid research which proves the complete opposite.
Is marijuana really worse than tobacco & alcohol?
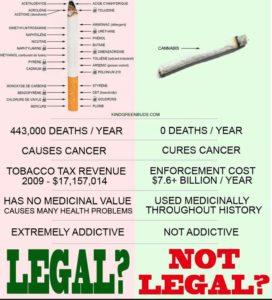
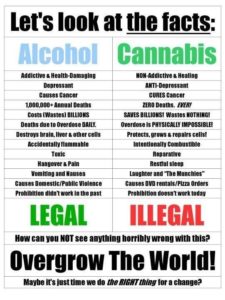
Another issue that’s worth throwing into the mix is the irony that tobacco and alcohol are, from a legal perspective, regarded as perfectly okay.
The following graphics give pause for thought if we want to attack marijuana. Both drinking alcohol and smoking tobacco are legal (for adults) but are reported to be responsible for what might be regarded as an unacceptable number of deaths every year. And this isn’t taking into account everything else associated with their use: all the workdays lost through illness/accidents; the personal pain and suffering for the smoker/drinker themselves; the knock-on pain and suffering of their loved ones; the financial cost of the products themselves over a lifetime of use; let alone the complete lack of proven health benefits weighed up against the wealth of proven health deficits associated with both of these substances.
Deaths association with tobacco vs marijuana
Alcohol vs Marijuana
Is marijuana a gateway drug?
For me, the view expressed by the NIH (the USA’s National Institute on Drug Abuse) 31 sums up the confusion in this area.
On the one hand, they say that some research 32 33 suggests: “…marijuana use is likely to precede use of other licit and illicit substances and the development of addiction to other substances.”
While, on the other hand, they state: “However, the majority of people who use marijuana do not go on to use other, “harder” substances. Also, cross-sensitization is not unique to marijuana. Alcohol and nicotine also prime the brain for a heightened response to other drugs 34 and are, like marijuana, also typically used before a person progresses to other, more harmful substances.”
Because of this lack of definitive research data, I can’t form any definitive opinion on this matter. I can say that I have personally known marijuana consumers who would fit into both categories – one has smoked marijuana all his life and has never, to my knowledge, progressed to stronger drugs, while another started with marijuana and ended up taking heroin and dying of throat cancer, possibly linked to the amount of tobacco and/or marijuana smoked during his relatively short life.
Final Thoughts
I don’t want to persuade anyone to start taking drugs. Indeed, I consider that a lot of the medical conditions that may be aided with the use of marijuana (from depression through to migraines, joint pain to MS and even cancer) are largely preventable through dietary and lifestyle choices alone. Thus cutting out the need for most prescriptions, including opioids and marijuana itself.
Also, I’ve come across some negative effects of marijuana-use in people I’ve known; thus, for me, there’s no hint of trying to push for legalisation per se. However, I think that, as with research into nutrition, the factual findings of reputable, peer-reviewed research into anything (including the potential medical effects of marijuana) should be the deciding factors in government/medical policies – and not the potentially biased opinions of legislators, funded and controlled by interested parties such as Big Pharma and the like.
Dr Greger’s Video on the above subject
References
- Marijuana Legalization & the Opioid Epidemic. Michael Greger M.D. FACLM June 22nd, 2018 Volume 42 [↩]
- Hurd YL. Cannabidiol: swinging the marijuana pendulum from ‘weed’ to medication to treat the opioid epidemic. Trends Neurosci. 2017;40(3):124-127. [↩]
- Cannabis Cannabinoid Res. 2017; 2(1): 160–166. Cannabis as a Substitute for Opioid-Based Pain Medication: Patient Self-Report. Amanda Reiman, Mark Welty, and Perry Solomon [↩]
- ScienceDaily: Medical marijuana could reduce opioid use in older adults. May 1, 2018. Northwell Health. [↩]
- Maida V, Daeninck PJ. A user’s guide to cannabinoid therapies in oncology. Curr Oncol. 2016;23(6):398-406. [↩]
- Hall W. U.S. policy responses to calls for the medical use of cannabis. Yale J Biol Med. 2015;88(3):257-264. [↩]
- Marijuana as Medicine? The Science Beyond the Controversy. Mack A, Joy J. Washington (DC): National Academies Press (US); 2000. [↩]
- Institute of Medicine. 1999. Marijuana and Medicine: Assessing the Science Base. Washington, DC: National Academy Press, p. 141. [↩]
- Clin Pharmacol Ther. 1977 Jan;21(1):26-33. Effects of intravenous tetrahydrocannabinol on experimental and surgical pain. Psychological correlates of the analgesic response. Raft D, Gregg J, Ghia J, Harris L. [↩]
- Jain AK, Ryan JR, McMahon FG, Smith G. 1981. “Evaluation of intramuscular levonantradol and placebo in acute postoperative pain.” Journal of Clinical Pharmacology 21:320S-326S. [↩]
- Noyes R Jr, Brunk SF, Baram DA, Canter A. 1975a. “Analgesic effect of delta-9-tetracannabinol.” Journal of Clinical Pharmacology 15:139-143. [↩]
- Noyes R Jr, Brunk SF, Baram DA, Canter A. 1975b. “Analgesic effect of delta-9-tetracannabinol and codeine.” Clinical Pharmacology and Therapeutics 18:84-89. [↩]
- Staquet M, Gantt C, Machin D. 1978. “Effect of a nitrogen analog of tetrahydrocannabinol on cancer pain.” Clinical Pharmacology and Therapeutics 23:397-401. [↩]
- ASCPT: Clinical Pharmacology. Effect of a nitrogen analog of tetrahydrocannabinol on cancer pain. M. Staquet C. Gantt D. Machin. April 1978. [↩]
- Consroe P, Musty R, Rein J, Tillery W, Pertwee RG. 1997. “The perceived effects of smoked cannabis on patients with multiple sclerosis.” European Neurology 38:44-48. [↩]
- Dunn M and Davis R. 1974. “The perceived effects of marijuana on spinal cord injured males.” Paraplegia 12:175. [↩]
- El-Mallakh RS. 1987. “Marijuana and migraine.” Headache 27:442-443. [↩]
- Wikipedia: THC or Tetrahydrocannabinol definition. [↩]
- Marijuana As Medicine?: The Science Beyond the Controversy Paperback – 30 Nov 2000 by Alison Mack [↩]
- Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med. 2014;174(10):1668-1673. [↩] [↩]
- Piper BJ, Dekeuster RM, Beals ML, et al. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol (Oxford). 2017;31(5):569-575. [↩]
- Socías ME, Kerr T, Wood E, et al. Intentional cannabis use to reduce crack cocaine use in a Canadian setting: A longitudinal analysis. Addict Behav. 2017;72:138-143. [↩]
- Abrams DI. Integrating cannabis into clinical cancer care. Curr Oncol. 2016;23(2):S8-S14. [↩]
- Wikipedia: Cannabinoids [↩]
- Blood Vessels on the Menu [↩]
- Wikipedia: Metastasis [↩]
- American Medical Association House of Delegates. AMA Resolution: 907(1-16). [↩]
- Hayes MJ, Brown MS. Legalization of medical marijuana and incidence of opioid mortality. JAMA Intern Med. 2014;174(10):1673-1674. [↩]
- Bradford AC, Bradford WD. Medical Marijuana Laws Reduce Prescription Medication Use In Medicare Part D. Health Aff (Millwood). 2016;35(7):1230-1236. [↩]
- Dyer O. US states that allow medical marijuana see drop in prescriptions for other drugs, study finds. BMJ. 2016;354:i3942. [↩]
- NIH National Institute on Drug Abuse: Marijuana – Is marijuana a gateway drug? [↩]
- Secades-Villa R, Garcia-Rodríguez O, Jin CJ, Wang S, Blanco C. Probability and predictors of the cannabis gateway effect: a national study. Int J Drug Policy. 2015;26(2):135-142. doi:10.1016/j.drugpo.2014.07.011. [↩]
- Weinberger AH, Platt J, Goodwin RD. Is cannabis use associated with an increased risk of onset and persistence of alcohol use disorders? A three-year prospective study among adults in the United States. Drug Alcohol Depend. February 2016. doi:10.1016/j.drugalcdep.2016.01.014. [↩]
- Levine A, Huang Y, Drisaldi B, et al. Molecular mechanism for a gateway drug: epigenetic changes initiated by nicotine prime gene expression by cocaine. Sci Transl Med. 2011;3(107):107ra109. doi:10.1126/scitranslmed.3003062. [↩]