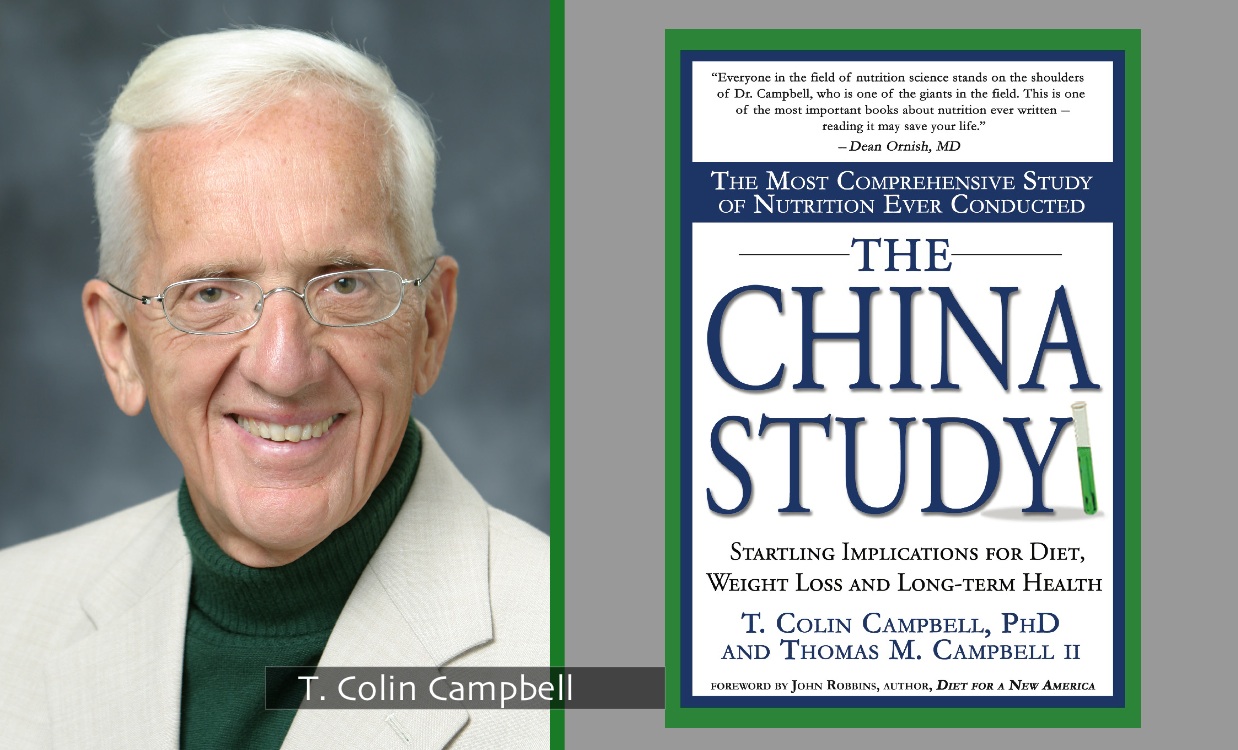
If you already know about The China Study then you will know how important a milestone it is for nutritional research. It’s such an important study that I thought it would be worth taking a quick look at its background, method and conclusions.
Background
Protein Consumption in Rats
Professor T Colin Campbell observed a relationship between the amount of dietary protein consumed and the promotion of cancer in rats. The animal protein used was casein (the main protein in milk and cheese), along with a variety of plant proteins. Distinct differences between the effects of animal vs. plant-based protein were observed:
- animal protein tended to promote disease conditions
- plant protein tended to have the opposite effect
Early 1970’s in China
The Chinese premier Zhou Enlai was dying of cancer. He had organised a survey called the Cancer Atlas which gathered details on about 880 million people. The survey revealed cancer rates across China to be geographically localised, suggesting dietary/environmental factors—not genes—accounted for differences in disease rates.
1983-1984 Survey
Dr. Campbell with researchers from Cornell University, Oxford University, and the Chinese government, conducted a major epidemiological study (i.e. a study of human populations to discover patterns of disease and the factors that influence them). This was called The China Project (from which the book The China Study derived some of its data). Researchers investigated the relationship between disease rates and dietary/lifestyle factors across the country.
Why China?
- large population of almost one billion
- very little migration within China
- rural Chinese mostly lived where they were born
- strict residential registration system existed
- food production was very localised
- the Cancer Atlas had revealed diseases were localised and so dietary and environmental factors (not genes) would be likely to account for disease rate variation by area (whether affluent and eating Western diet, or rural and eating traditional plant-based diet)
Method
Research Questions
1. Is there an association between environmental factors, like diet and lifestyle, and risk for chronic disease?
2. Would the patterns observed in a human population be consistent with diet and disease associations observed in experimental animals?
Hypothesis
Researchers hypothesised generally that an association between diet/lifestyle factors and disease rates would indeed exist. A specific hypothesis was that animal product consumption would be associated with an increase in cancer and chronic, degenerative disease.
Hypothesis Testing
6,500 adults in 65 different counties across China were surveyed in the 1983-4 project. These counties represented the range of disease rates countrywide for seven different cancers. The survey process with each participant included:
- three-day direct observation
- comprehensive diet and lifestyle questionnaires
- blood and urine samples
- food samples from local markets analysed for nutritional composition
- survey of geographic factors
1989-1990 Survey
- same counties and individuals resurveyed plus a survey of 20 additional new counties in mainland China and Taiwan.
- 10,200 adults surveyed
- socioeconomic information collected
- data combined with new mortality data for 1986-88
Analysis of Data from both 1983-1984 & 1989-1990 Surveys
- data was analysed at approximately two dozen laboratories around the world to reduce chances of error in data analysis
- researchers could be confident that if results were consistent, then they would be correct
Conclusion
- diseases more common in Western countries clustered together geographically in richer areas of China
- diseases in richer areas of the world were thus likely to be attributed to similar “nutritional extravagance”
- diseases in poorer areas of the world were likely to be attributed to nutritional inadequacy/poor sanitation
- blood cholesterol (strongly associated with chronic, degenerative diseases) was higher in those consuming more animal foods
- lower oestrogen levels in women (associated with fewer breast cancers) related to increased plant food consumption
- higher intake of fibre (found only in plants) associated with lower incidence of colon and rectal cancer
The consistency of the results led the researchers to make the overall conclusion that the closer people came to an all plant-based diet, the lower their risk of chronic disease.
Published Data
- The data on both the 1983-1984 survey and the 1989-1990 survey can be seen in more detail here.
- More detail on the experimental study design of the China Project (covered in Appendix B) plus a full copy of The China Study in pdf format is available here.
- Professor T Colin Campbell’s complete CV (including published papers analysing data from the China Project) is available here.
Plant Protein vs Animal Protein Webinar from Professor T Colin Campbell
If you have any comments or require further information on this topic, please let me know.
Bibliography:
- Chen J, Campbell TC, Li J, Peto R. Diet, Life-Style and Mortality in China: A Study of the Characteristics of 65 Chinese Counties. Oxford, UK: Oxford University Press; 1990.
- Chen J, Peto R, Pan W-H, Liu B-Q, Campbell TC, Boreham J, Parpia B. Mortality, Biochemistry, Diet and Lifestyle in Rural China: Geographic Study of the Characteristics of 69 Counties in Mainland China and 16 Areas in Taiwan. Oxford, UK; Ithaca, NY; Beijing, PRC: Oxford University Press, Cornell University Press; People’s Medical Publishing House, 1990.