An April 2019 UK study 1 looked at the sort of food, drink and lifestyle choices made by meat-eaters and plant-eaters to see if differences in health outcomes of the two groups were partly the result of these choices.
The study
The researchers analysed data from FFQs (food frequency questionnaires) completed by 30,239 participants involved in the EPIC-Oxford study 2 . They assessed intakes of major protein-source foods and other food groups after dividing the participants into six groups of meat-eaters and non-meat-eaters:
- regular meat-eaters
- low meat-eaters
- poultry-eaters
- fish-eaters
- vegetarians
- vegans
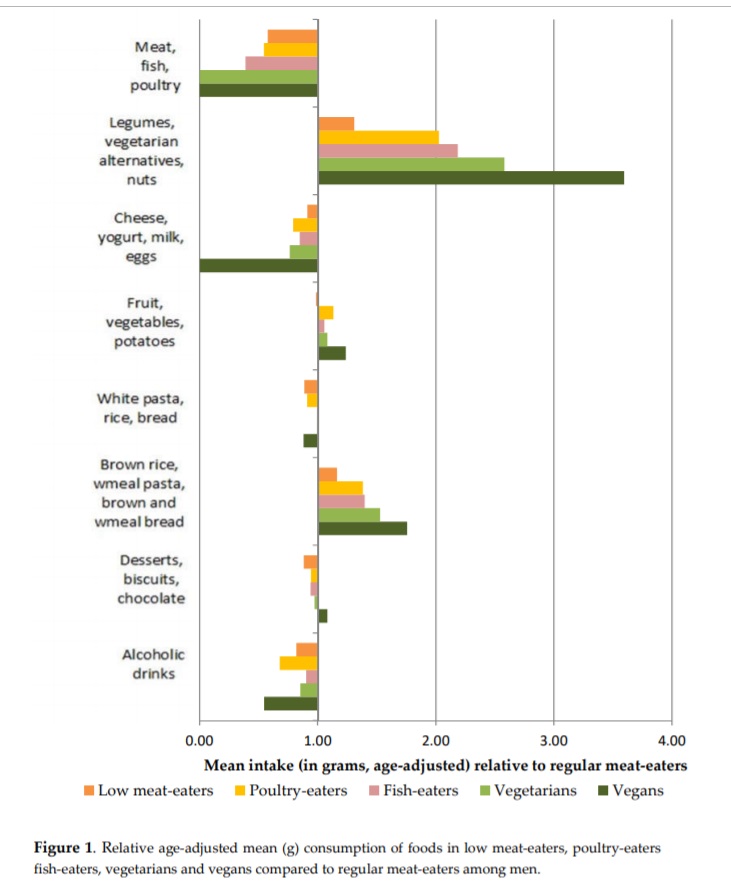
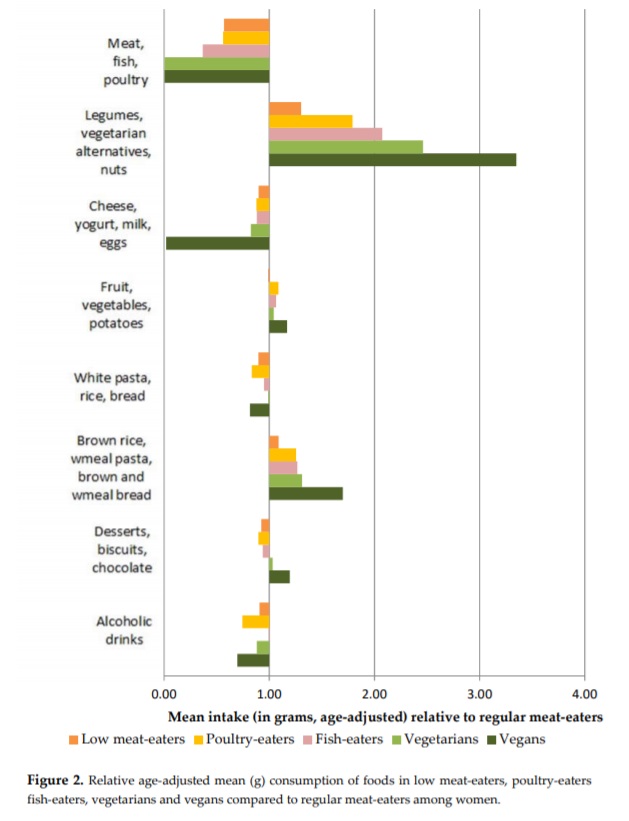
The foods listed in the FFQs were categorised into 45 food groups and the results were analysed for variance in health outcomes between the 6 groups. Figures 1 (men) and 2 (women) give a rough idea of the results:
Study findings
There are large differences in dietary intakes between meat-eaters and non-meat-eaters:
non-meat-eaters consumed higher amounts of:
- soy
- legumes
- pulses
- nuts and seeds
- whole grains
- vegetables and fruits
non-meat-eaters consumed lower amounts of:
- refined grains
- refined carbohydrates
- fried foods
- alcohol
- sugar-sweetened beverages (SSBs)
- other foods high in free sugars (e.g. ice cream)
Contrary to expectations, vegetarians and vegans did not replace meat with higher intakes of animal-sourced protein alternatives (dairy and eggs) and non-animal protein alternatives (including legumes and nuts), respectively.
Vegetarians and vegans were found not to completely replace meat consumption with non-meat protein sources and high protein plant-sources but, rather, they increased their consumption of a large variety of plant-based foods and consumed lower amounts of high protein-sourced foods compared with meat-eaters.
The positive health benefits of lower protein intake (specifically, animal protein) have been discussed previously 3 4 5 6 .
The proportion of total energy from high protein-sourced foods:
- regular meat-eaters – 33%
- vegetarians – 25%
- vegans – 20%
Compared with the 5 other groups, vegans consumed the highest amount of:
- plant milk
- nuts
- brown rice
- wholemeal pasta
- couscous
- wholemeal bread
Vegetarians consumed:
- lower amount of dairy and eggs than meat-eaters
- highest amount of cheese compared with other 5 groups
Egg consumption was low in all 6 groups, possibly because this study looked at a cohort that might be more ‘health conscious’ than the rest of the population. 7
Compared with regular meat-eaters, all the other groups:
- were younger
- had a higher education level
- had a lower socio-economic status
- were less likely to smoke and consume alcohol
- had higher levels of physical activity
- had lower BMI
- had higher intakes of carbohydrates
- had lower intakes of protein and fat
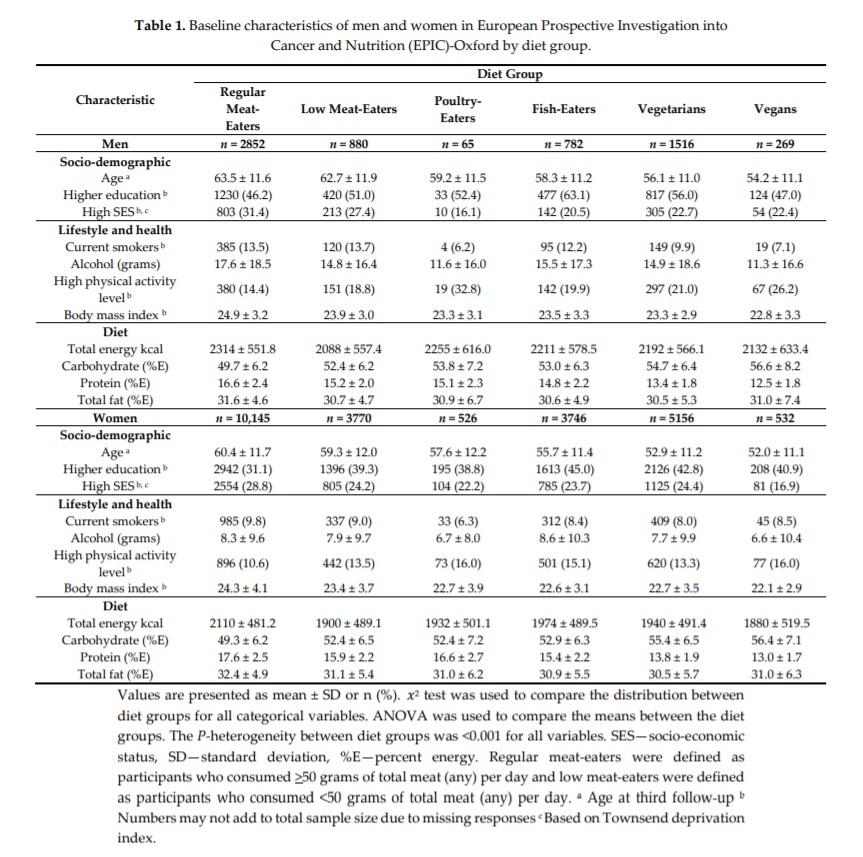
Table 1 shows more detail on the above:
Study conclusions
The findings suggest that non-meat-eaters might be consuming an overall “healthier” diet than meat-eaters.
“In this large study of British men and women, we compared intakes of major protein-source foods and other food groups. …Our results show that meat-eaters and low and non-meat-eaters do not only differ in their meat consumption but in their overall dietary intake…The dietary intakes consumed by low and non-meat-eaters might explain the lower risk for some diseases in these diet groups and can be used as a real-life guide for future work assessing the health impacts of replacing meat intake with plant-based foods or dietary recommendations.”
Final thoughts
On the whole, the results are what one would have expected. However, there were some surprises, particularly the findings that non-meat eaters tend to drink less booze, smoke less, and eat less processed and sweetened foods.
It’s often speculated, by those who are unfamiliar with plant-based diets, that life must be more boring when you stop eating animals – I mean, where’s the fun in eating grass?! However, if life were so dull when eating a supposedly buzz-free diet, wouldn’t you imagine that plant-eaters would eat a lot more comfort food 8 (sugary, fried, processed foods) and drink and/or smoke themselves silly whenever they could?
Some clarification is provided by research data showing that, not only does physical health generally improve on a plant-based diet, but mental health 9 10 11 and general outlook on life 12 also tends to improve – obviating the need to get caught in that “pleasure trap” 13 .
It was also interesting to note from this study, that the improved health outcomes for plant-eaters does not just derive from the fact that they eat more healthy foods – it’s also that they generally appear to eat less unhealthy food, exercise more, smoke and drink less. There was also variance by age, socio-economic and educational status between the groups – with the youngest group being vegan, highest socio-economic status being meat-eaters, and the most educated being fish-eaters. Food for thought…
Of course, this is not to say that there are no vegetarians and vegans eating horrendously unhealthy plant-based diets. This is something that’s been covered in previous blogs 14 15 16 . This can probably be seen by the surprisingly low amount of fruit and veg eaten by vegetarians and vegans, when compared with how much rice, pasta and bread they eat.
Since WFPB (especially when non-SOS) would guarantee a maximum amount of fruit and veg, with a minimum amount of the sort of junk foods that can find themselves included in a vegetarian or vegan diet, it would be interesting to see future studies which are able to include the WFPB diet within a list of food groups.
References
- Comparison of Major Protein-Source Foods and Other Food Groups in Meat-Eaters and Non-Meat-Eaters in the EPIC-Oxford Cohort. Papier K, Tong TY, Appleby PN, Bradbury KE, Fensom GK, Knuppel A, Perez-Cornago A, Schmidt JA, Travis RC, Key TJ. Nutrients. 2019 Apr 11;11(4). pii: E824. doi: 10.3390/nu11040824. [↩]
- European Prospective Investigation into Cancer and Nutrition (EPIC)-Oxford study [↩]
- The Problem with Protein [↩]
- Eat Enough Food & You Eat Enough Protein [↩]
- Animal Protein & Your Kidneys [↩]
- Plant Protein, Fibre & Nuts Lower Cholesterol & Blood Pressure [↩]
- Sobiecki, J.G.; Appleby, P.N.; Bradbury, K.E.; Key, T.J. High compliance with dietary recommendations in a cohort of meat eaters, fish eaters, vegetarians, and vegans: Results from the European Prospective Investigation into Cancer and Nutrition–Oxford study. Nutr. Res. 2016, 36, 464–477. [↩]
- Ghrelin & Obesity – A Tentative Step Through the Minefield [↩]
- Depression is Linked to Inflammation [↩]
- Gut Microbiota & Depression [↩]
- Depression & IBD / Crohn’s Disease / Ulcerative Colitis [↩]
- What’s the Psychology of Plant-Eaters? [↩]
- Bliss Points, Pleasure Traps & Wholefood Plant-Based Diets [↩]
- Greggs’ Vegan Sausage Rolls – Why Veganism Can Fail [↩]
- Vegan Pie Comes Top in British Pie Awards 2019 [↩]
- Vegan Burgers – Healthy & Yum Yum? Forget it! [↩]

 Vitamin B12 acts as a
Vitamin B12 acts as a